CHAPTER 3 Evaluation and Selection of the Implant Patient
INTRODUCTION TO PATIENT SCREENING AND MEDICAL EVALUATION
Implant dentistry has progressed amazingly during the past 20 years. Every aspect, whether scientific or clinical, is taught in academic institutions around the world with a discipline and demands equal to those of other types of surgical instruction. However, one vital element that has been underemphasized is the meticulous physical evaluation of patients before, during, and after implant treatment. This element is becoming increasingly important because, as mentioned previously, life expectancy in the industrialized nations is increasing, and a growing number of elderly patients will have implant-supported prostheses.
Absolute Contraindications
Absolute contraindications arise from health conditions that may jeopardize the patient’s overall health and seriously compromise the survival of implanted systems, resulting in residual chronic complications (Table 3-1).
Table 3-1 Systemic Absolute Contraindications to Implant Surgery and Their Impact on Predictability
| Health Condition | Risks for Patient’s General Health | Severity of Immediate Implant Complications | Long-Term Predictability of Implant System |
|---|---|---|---|
The number of + relates to the degree of gravity of the complications associated with implant and graft surgery. One + is the least complicated (least predictable), and four ++++ is the most complicated (most predictable). Zero corresponds to total unpredictability.
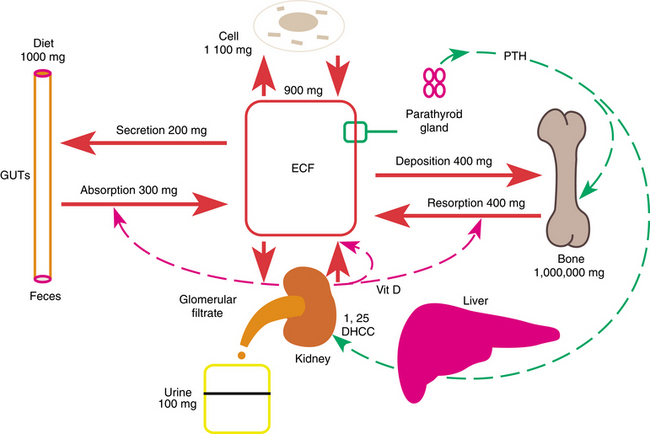
Fig. 3-1 illustrates daily calcium metabolism. The kidneys initially filter about 10 g of calcium a day into the primary urine.
Relative Contraindications
Patient selection with regard to relative contraindications is much more subtle, and among all the criteria, the dental practitioner’s judgment remains the critical factor. If the practitioner is not medically oriented, the patient may need to be referred to a specialist. If a disorder has been adequately corrected, the dental practitioner can carry out the treatment plan; otherwise, treatment should be postponed until optimal conditions prevail. Table 3-2 presents the possible effects of relative contraindications on the success of implant and bone graft surgery.
Table 3-2 Systemic Relative Contraindications to Implant Surgery and Their Impact on Predictability
| Health Condition | Risks for Patient’s General Health | Long-Term Implant Predictability in Absence of Proper Diagnosis or Treatment | Patient’s Possible Response to Medical Treatment Before Implant Surgery | Long-Term Implant Predictability After Proper Diagnosis and Treatment |
|---|---|---|---|---|
(2) ++
++
++
+++
The number of + relates to the degree of gravity of the complications associated with implant and graft surgery. One + is the least complicated (least predictable), and four ++++ is the most complicated (most predictable). Zero corresponds to total unpredictability.
Modern chemotherapy uses a wide range of drugs, which belong to 10 to 12 pharmacologic families. Treatment for each patient may include a complex combination of these drugs. Table 3-3 shows the principal cancer treatments that may present absolute contraindications to an implant procedure during the time they are administered or for up to 6 months thereafter. Table 3-2 also shows a proportionately limited number of drugs that are incompatible with the simultaneous insertion of implant devices. The interpolating agents on the whole, seem to be devoid of adverse effects on implantology. The interferons and interleukins prescribed in advanced stages of pathology, however, are particularly contraindicated.
Table 3-3 Effects of Chemotherapeutic Drugs on Critical Metabolic Functions
| Type of Anticancer Drug or Agent | Drug Family | Commercial Brand | Principal Complications, Disorders, or Affected Organs |
|---|---|---|---|
| Antifolic | Methotrexate | Thrombopenia, osteogenesis | |
| Nitrogen-mustards (III) Nitrogen-urea (IV) Mitomycin |
Ifosfamide Streptozocin Ametycin |
Blood, bone (osteogenesis) Renal, hepatic, blood Renal, hepatic, blood |
|
| Vinca alkaloids (III) | Vincristine | Renal, hepatic, blood | |
| N/A | N/A | N/A | |
| Bleomycin | Bleomycin | Pulmonary fibrosis | |
| Plicamycin | Mithramycin | Renal, hepatic, blood (Ca)++ |
|
| Progestates | Medroxyprogesterone Ethynodiol |
Renal, hep/> |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses