Trauma, burns and abuse
Key Points
This chapter deals with: trauma to the head, maxillofacial area and spine; burns; gunshot and stab wounds; and human bites. Animal bites, sports injuries and child abuse are discussed elsewhere (Chs 25 and 33).
General Aspects
Injuries outrank cancer and heart disease as a leading cause of death in children, and in men up to the age of 35. It is males predominantly who are affected by trauma. Up to a third of these deaths are, theoretically, preventable. Violence (assaults or fights; Figs 24.1–24.3) and road traffic accidents are the major causes of trauma, with alcohol or other drugs being frequent cofactors. In the Western world, assaults are increasingly common but, in contrast, trauma from road traffic accidents (RTAs) has become less common since the institution of seatbelt-wearing. Nevertheless, 3500 people are killed and 40 000 seriously injured each year from RTAs in Britain. Maxillofacial trauma is the single most common injury to occupants of vehicles involved in RTAs, even in seatbelted drivers. Airbags may be a supplemental restraint system but they themselves can cause injury – particularly in people of short stature, unrestrained or out of position within the vehicle. Industrial accidents, sport, falls, epilepsy and non-accidental injuries (child abuse) are other causes of trauma. Equine-related maxillofacial fractures mainly involve the young and predominantly females, and alcohol is rarely implicated.



The main causes of oral and craniofacial injuries are sports, violence, falls and RTAs. Cranial injuries are a leading cause of mortality and oral–facial injuries can result in disfigurement and dysfunction, greatly diminish quality of life and cause social and economic burdens.
Sports
Craniofacial sports injuries arise mainly in contact sports, but also in activities such as cycling, skating and gymnastics, especially on trampolines (Ch. 33).
Violence
Domestic violence, including child abuse, spousal and elder abuse, and abuse of the disabled, is the single most common type of violence. Child abuse is of particular concern (Ch. 25) because more than 65% of cases involve head and oral–facial trauma, and in the young child, head injury is the most common cause of death. Dentists are required to report suspected cases. The incidence of specific injury patterns and outcomes of violence in adults are similar between the genders. Males, however, make up the majority of facial fracture cases (over 70%); the aetiology of their injuries includes altercations with strangers, often after consuming alcohol or using drugs, or violent gang activities. Males are more likely to be admitted with fracture but not soft-tissue injury only; more likely to be assaulted with a weapon; and more likely to be involved in an altercation, gang violence, arrest or robbery. Females are more prone to domestic violence and rape, and less likely to be involved in violent criminal activity or to have gang associations. One in six women in the USA has been a victim of sexual violence (a completed or attempted rape) at some time in her life.
Falls
Falls are a major cause of trauma to face, jaws and teeth in adults and children. Orofacial injuries are common from toddlers falling with a bottle, dummy or sippy cup in their mouth; bottles are most likely to be the source of injury, followed by dummies and sippy cups. Injuries consist mainly of mouth lacerations. Falls may indicate underlying pathology or simple locomotor inadequacy and are especially common after the age of 80 years. In old people, it is important to establish whether they are prone to falls, which may need further investigation. Important individual risk factors include:
Road traffic accidents
The effects of RTAs may range from minor and reversible effects to long-term medical, surgical and rehabilitative consequences. Post-traumatic headaches and chronic oral–facial pain is not uncommon. Whiplash-associated disorders (WADs) can lead to temporomandibular pain, predominantly in females. Neuromuscular and glandular damage may cause problems with chewing, swallowing and tearing – or result in facial tics or paralysis.
Craniofacial trauma
In conflicts, assaults and RTAs, injuries often involve multiple organs. Death may result immediately from trauma, especially if there is head injury and brain damage, airway obstruction or damage to the spine and other vital organs (e.g. heart or liver).
Head Injuries
Head injuries are present in about 70% of patients admitted with multiple injuries, and about 3% of multiply injured patients have intracranial haemorrhage. Most head injuries are in previously fit young males because of their risk behaviour: RTAs and assaults are major causes (Fig. 24.4). Children and adolescents can sustain head injuries during sports or fights, and young children, particularly before they have perfected their walking skills, are also uniquely susceptible to head trauma because of higher cranial mass to body ratio.

Head injuries are a major cause of death – almost 50% of which happen before the patient reaches hospital – and most of the remaining deaths follow within the first few hours. Of those with brain injury, 12% die within 2 days. It is important to appreciate that the brain can be fatally damaged without fracture of the skull or even a blemish on the scalp.
Immediate Care
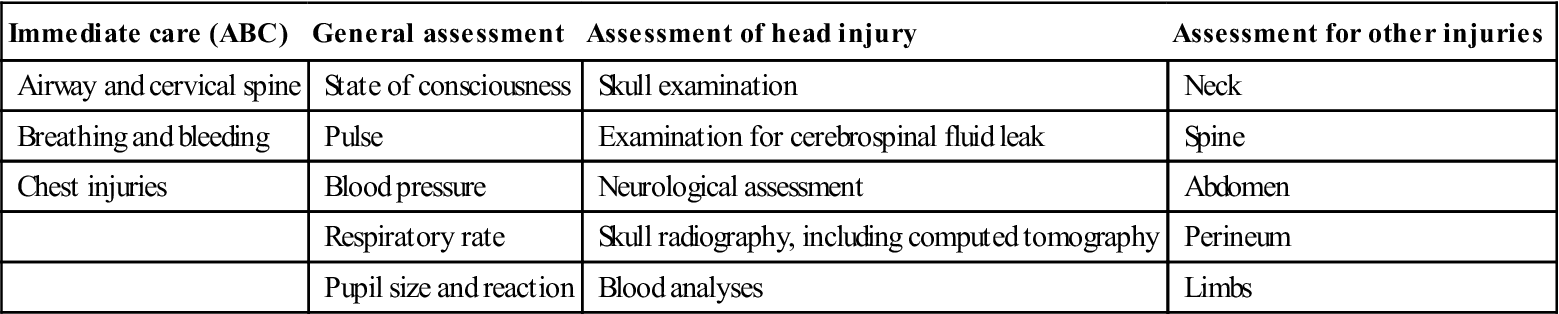
Damage to the head, cervical spine, chest, liver or spleen can be immediately life-threatening. In particular, there can be hazards to the airway; damage to the cervical spine; severe haemorrhage; and damage to kidneys or bladder or to other bones. All patients with head injuries must be urgently assessed using the ABC system: airway and cervical spine, breathing and bleeding, and chest injuries (Table 24.1).
Table 24.1
Head injuries: initial and early management
< ?comst?>
| Immediate care (ABC) | General assessment | Assessment of head injury | Assessment for other injuries |
| Airway and cervical spine | State of consciousness | Skull examination | Neck |
| Breathing and bleeding | Pulse | Examination for cerebrospinal fluid leak | Spine |
| Chest injuries | Blood pressure | Neurological assessment | Abdomen |
| Respiratory rate | Skull radiography, including computed tomography | Perineum | |
| Pupil size and reaction | Blood analyses | Limbs |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Airway establishment and maintenance has the highest priority. Respiratory obstruction is the most important preventable cause of early death and may be due to several causes, such as those shown in Box 24.1. Many patients have died from neglect of the airway before admission to hospital. Foreign bodies or the tongue can easily fall back to obstruct respiration, especially if there are bilateral fractures or comminution of the mandible, and the patient is unconscious. There is special danger to the airway if there has been trauma to and oedema of the tongue, fauces, pharynx or larynx, or uncontrollable nasoethmoidal haemorrhage.
Severely injured patients must have their airways (mouth and pharynx) cleared of debris and sucked out using direct vision and strong suction; they should be laid semi-prone on their side, face towards the ground, to allow any potential obstruction to fall forwards. Great care must be taken to avoid further neurological damage if a cervical spine injury is suspected. In the case of bilateral mandibular body fractures, a traction suture through the tongue will hold it forward; frequently, however, medial displacement of the posterior fragments prevents the anterior fragment from falling backwards unless the bone is comminuted. Posterior displacement of the maxilla in middle third injuries may cause the soft palate to occlude the airway. Obstruction can then be overcome by manual disimpaction of the maxilla. In the unconscious patient, a cuffed endotracheal tube may be needed to maintain the airway.
Should these non-invasive manœuvres fail to relieve obstruction immediately, a surgical airway, using endotracheal intubation or cricothyroidotomy, must be made. If there is supraglottic airway obstruction, a temporary airway can be established by laryngotomy using a wide-bore (2–3-mm) needle inserted through the cricothyroid membrane. In certain laryngotracheal crush injuries and other wounds that transect the trachea, it may be necessary to perform emergency tracheostomy (Fig. 24.5) or occasionally submental intubation. Indications for tracheostomy are summarized in Table 24.2.

Table 24.2
| What is obstructing the airway | Where positive pressure ventilation is needed | Where tracheobronchial suction is needed |
| Gross retroposition of the middle third of the face | Crushed or flail chest | Chronic obstructive pulmonary disease |
| Pharyngeal oedema | Prolonged mechanical ventilation | |
| Uncontrollable nasal haemorrhage | ||
| Loss of tongue control | ||
| Cancer surgery |
Chest injuries, particularly those causing tension pneumothorax or flail chest, or those caused by inhalation of toxic or hot gases, further impair respiration (see Burns). Flail chest can be recognized by extreme difficulty in breathing, associated with paradoxical movements of the chest and cyanosis. Intermittent positive-pressure ventilation must be given via a cuffed endotracheal tube.
Cervical spine stabilization is extremely important since injury is possible, especially in patients with injury above the clavicles or head injury resulting in an unconscious state, or any injury produced by high speed. Cervical spine injury is potentially fatal and may be symptomless whilst the patient is conscious due to protective muscle spasm that ‘stabilizes’ the spine; GA is very dangerous, as this protective muscle spasm is abolished on induction. Features can include neurological deficit and neck pain. Avoid any movement of the spinal column, and establish and maintain proper immobilization with the use of an appropriate neck splint until vertebral fractures or spinal cord injuries have been carefully ruled out with lateral cervical spine radiographs and computed tomography (CT).
Haemorrhage must be controlled. External bleeding is managed by direct pressure over any bleeding site until permanent control can be achieved by clamping and ligation. Shock due to bleeding that has led to hypovolaemia should be prevented or controlled and organ perfusion ensured by using intravenous fluid replacement (Ringer’s lactate, normal saline or blood transfusion). Vital signs should be monitored closely.
Severe haemorrhage or shock only rarely results from isolated head injuries or maxillofacial trauma, unless caused by gunshot wounds, so if such a patient is shocked, it is essential to exclude other injuries (damage to internal organs or fractures of the pelvis or limbs). Remember that bleeding may be concealed or occasionally aggravated by disseminated intravascular coagulation (Ch. 8). Severe haemorrhage can lead to cardiac or renal failure or cause fatal cerebral hypoxia. Haemorrhage into the pleural cavity from fractured ribs can embarrass respiration.
Latent haemorrhage may be recognized by rising pulse rate, falling blood pressure, increasing pallor, air hunger or restlessness. If haemorrhage is suspected, a surgical opinion should be sought, a blood sample should be taken for grouping and cross-matching, and the following quarter- or half-hourly observations should be recorded:
Blood transfusion may be indicated but is not needed to replace loss of less than 500 mL in an adult, unless there was pre-existing severe anaemia or deterioration of the general condition warrants transfusion, since there are risks, such as from transfusion reactions, fluid overload and infection. Meanwhile, since time is needed to obtain correctly cross-matched blood, normal saline, plasma or a plasma expander, such as dextran 70 or 110, may be given initially. Dextrans or other plasma expanders, together with tranexamic acid or desmopressin, may be the only possibility for Jehovah’s Witnesses. Dextran can interfere with blood-grouping and cross-matching so that blood samples should be collected before a dextran infusion is started (Ch. 8).
Estimation of blood urea and electrolyte levels are needed in case there has been renal failure secondary to loss of blood, and as a baseline to monitor progress and the effects of intravenous fluid replacement. A full blood picture is also needed as a baseline for possible effects of transfusion and for any coincidental haematological disease. Early haemoglobin levels give no useful indication of the amount of blood lost, as haemodilution will not have had time to develop.
Blood and urine samples should be collected for analysis for alcohol, drugs and metabolic disorders, particularly diabetes. However, transient glycosuria unrelated to diabetes may follow the stress of head injuries.
The reader should consult the Advanced Trauma Life Support Manual and similar guides for full details on this important topic. A detailed assessment of maxillofacial injuries is only undertaken once the patient has been assessed and stabilized.
General Assessment
A good history must be obtained from the patient, if conscious, and witnesses. Reports of loss of consciousness, amnesia, nausea, vomiting or headache must be noted, as well as the medical history, especially use of drugs, including recreational agents or anticoagulants, or any history of epilepsy. A description of the mechanism of injury is useful, as it will give a clue as to what injuries to exclude. Family or friends may help with the patient’s medical background.
Conscious State
Many patients are confused, concussed or comatose following head injury, though 30% of those with ultimately fatal head injuries may talk after injury and some are completely lucid for a time. However, the brain is invariably damaged in those who have lost consciousness for however brief a period, and sometimes in those who have not. Amnesia is common. Many are also suffering effects of alcohol or other drugs.
Maintenance of consciousness does not guarantee the absence of brain injury but the extent of retrograde amnesia is a rough measure of its severity.
Concussion, an immediate but transient loss of consciousness, is always associated with a short period of amnesia, and there is some brain damage even if after-effects are not detectable on neurological testing, cerebrospinal fluid (CSF) examination, CT or magnetic resonance imaging (MRI). Although the patient may lose consciousness only transiently, consciousness is almost invariably impaired after diffuse brain damage, and there is usually amnesia for the traumatic event, and afterwards (post-traumatic amnesia) for a period far exceeding that of coma. Consciousness may not be lost if brain damage is local, when, for example, the skull is penetrated by a sharp object.
Prolonged unconsciousness, when there are no complications such as brain haematomas and where there are no focal signs, is often caused by severe brain damage but sometimes by drugs (Table 24.3).
Table 24.3
| Brain lesions | Main causes |
| Cerebral cortex damage | Trauma, haemorrhage, hypoglycaemia, hypoxia, infection |
| Brainstem compression | Various |
| Brainstem localized pressure | Cerebellar haemorrhage, abscess, neoplasm |
| Brainstem reticular activating substance suppression | Drugs (alcohol and others) |
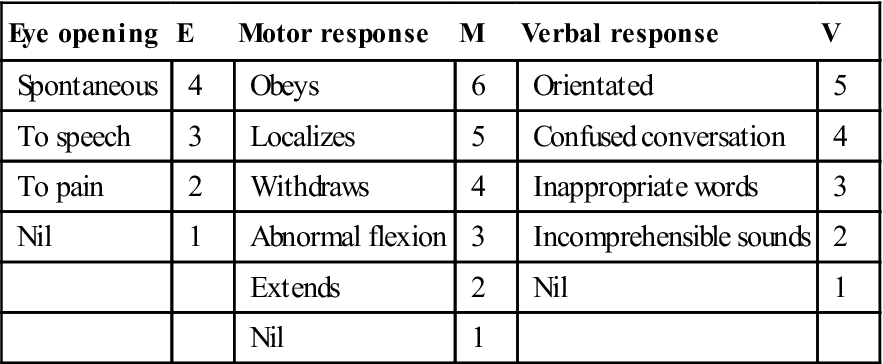
The most essential examination is immediately to assess, record and monitor the level of consciousness using the Glasgow Coma Scale (GCS), which scores points derived from three features: eye opening (E); motor response (M); and verbal response (V) (EMV score; Table 24.4). The degree of brain damage is initially assessed by the level of consciousness as measured by the GCS and, later, by the duration of coma and post-traumatic amnesia. It is important to consider causes of coma other than acute head injury (see Appendix 24.1). The EMV score or responsiveness sum can range from 3 to 15. A fully alert and otherwise well patient with a full and unchanging score of 15 and no neurological signs or symptoms and no skull fracture or intracranial haemorrhage on CT or MRI scan does not need hospital admission for observation, unless for other reasons. All patients who score below 15 points (see Table 24.4) should be admitted to hospital for observation – even if drugs or alcohol are the suspected causes. A score of 7 or less indicates coma in 100%; 9 or more indicates absence of coma. Patients with a GCS score of less than 8 require immediate neurosurgical attention (Table 24.5). About 85% of patients with a score of 3 or 4 succumb within 24 hours.
Table 24.4
Glasgow Coma or Responsiveness Scale (GCS)
< ?comst?>
| Eye opening | E | Motor response | M | Verbal response | V |
| Spontaneous | 4 | Obeys | 6 | Orientated | 5 |
| To speech | 3 | Localizes | 5 | Confused conversation | 4 |
| To pain | 2 | Withdraws | 4 | Inappropriate words | 3 |
| Nil | 1 | Abnormal flexion | 3 | Incomprehensible sounds | 2 |
| Extends | 2 | Nil | 1 | ||
| Nil | 1 |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Table 24.5
Indications for neurosurgical attention after head injury
| Immediate neurological attention indicated | Early neurological attention indicated | Admission to hospital for neurological observation |
| Glasgow Coma Scale score (GCS)<8 | GCS 8–14 | GCS<15 |
| Deteriorating consciousness | Convulsions | Minor skull fracturea |
| Neurological lateralization (pupillary inequality and hemiparesis) | Cerebrospinal rhinorrhoea or otorrhoea | Post-traumatic amnesia |
| Dilated fixed (unreactive to light) pupil | Orbital or retromastoid haematomas | Other serious injuries |
| Major skull fractures (depressed or compound) | Pneumoencephalocoele | Children |
| CT signs of compression or obliteration of mesencephalic cisterns, midline hemisphere shift, or one or more surgical masses | Worsening restlessness, headache and vomiting | Patients with psychiatric disease, drug abuse or learning impairment |
| Uncontrollable bleeding | Patients living alone or without a responsible adult companion | |
| Rising blood pressure with bradycardia |
aThere is some controversy among neurosurgeons about whether patients with skull fractures with no evidence of cerebrospinal fluid leak, cerebral haemorrhage or pneumoencephalocoele should receive observation or operative treatment.
It is important also to recognize and to treat other factors that can contribute to morbidity and mortality, which can include airway obstruction, hypotension, meningitis, uncontrolled epilepsy, stress-induced gastric bleeding or diabetic ketoacidosis.
Patients who survive with head injuries fall into three main groups. Most are stable neurologically with gradual improvement in consciousness. Some progressively deteriorate in the level of consciousness with localizing signs, often because of intracranial bleeding with or without cerebral oedema, when the bleeding usually needs to be evacuated by craniotomy. Others have rising intracranial pressure (ICP), causing progressive deterioration in consciousness in the absence of localizing signs. ICP should be monitored. Cerebral oedema management remains controversial but general measures include optimal head and neck positioning 30° to the horizontal for facilitating intracranial venous outflow, avoidance of dehydration and systemic hypotension, and maintenance of normothermia, while specific therapeutic interventions are controlled hyperventilation, administration of corticosteroids and diuretics, osmotherapy, and pharmacological cerebral metabolic suppression. Ensuring adequate oxygenation, giving furosemide and restricting fluid are common strategies.
Patients must be carefully and regularly observed to detect the development of complications, especially intracranial haematomas, which need immediate neurosurgical attention. The level of consciousness should be charted, as assessed by the GCS and, later, by the duration of coma and of post-traumatic amnesia; this should take place at regular intervals – half-hourly or even more frequently – along with measurements of pulse, blood pressure, respiration, pupil reactivity and temperature.
Deterioration of consciousness is the most important sign, and is sometimes accompanied by worsening restlessness, headache and vomiting. Fixed dilatation of the pupil on the side of the fracture and decerebrate rigidity – late signs caused by raised ICP and brain shift – are soon followed by bilateral pupil dilatation, periodic respiration, respiratory arrest and death, unless there is immediate neurosurgical intervention. Focal signs, such as hemiparesis, dysphasia or focal epilepsy, are uncommon. In deep coma there are no verbal or motor responses, but in less severe cases the eyes may open transiently from time to time and there may be vague or weak responses to stimuli.
Up to 60% of all patients admitted in coma are alcoholics or other drug users who have often had a head injury. Toxic and metabolic disorders cause no focal or localizing neurological signs, although some drug misuse (opiates) can affect pupil reactivity. When there is disease of the central nervous system (CNS) itself, sensory or motor disturbances may indicate the lesion site. In some of these diseases, white cells, bacteria or blood may also appear in the CSF. Intoxications, whether the result of exogenous agents or disorders of metabolism and severe infections, all have essentially similar effects and will not be discussed further.
The level of consciousness is depressed further by sedatives and many analgesics, especially morphine and its analogues, which not only slow respiration but also disguise eye signs of rising intracranial pressure, by causing pupillary constriction. Pentazocine is also contraindicated. If analgesia is essential, codeine, diclofenac or buprenorphine can be used. Benzodiazepines should not be given for controlling fits or to allow suturing, since they cause respiratory depression, which can be fatal unless ventilation is given. If there are repeated fits, phenytoin by intravenous infusion is less likely to depress respiration. Alcohol must be prohibited.
Pupil size and reaction must be checked for localizing signs of neurological damage. A dilated fixed (unreactive to light) pupil often indicates rising ICP and is usually a serious sign. Severe facial oedema may make examination of the eyes difficult and the eyelids should then be prised open. A fixed dilated pupil may also be caused by local damage to the optic or oculomotor nerves, and must be differentiated by clinical examination, radiographs (usually CT) and MRI, and by the absence of signs associated with brain damage or of rising ICP. Limb reflexes should be tested.
Regular monitoring of blood pressure and pulse rate is essential. A low or falling blood pressure with rising pulse rate is indicative of haemorrhage or shock, which can lead to fatal cerebral anoxia or renal failure. A systolic blood pressure of lower than 60 mmHg brings with it a risk of brain damage. A high or rising blood pressure with bradycardia, by contrast, is indicative of raised ICP secondary to cerebral oedema or haemorrhage as a result of the injury. Respiratory rate, urine output and fluid balance must also be monitored.
Assessment of Head Injury
Skull examination
Scalp lacerations may be associated with a fracture; they can cause severe loss of blood and provide a pathway for infection into the cranial cavity. The presence of a skull fracture greatly increases the risk of brain damage and an intracranial haematoma; significant intracranial lesions are found in two-thirds. A depressed skull fracture may be palpable, although it is often concealed by overlying oedema of the soft tissues. About 80% of skull fractures are linear, and many are associated with subepidural or epidural haematomas. Basal skull fractures are usually uncomplicated; they may not be visible on routine radiography but may be revealed by bleeding, which may show as haemotympanum (blood behind the ear drum), as ecchymosis over the mastoid process (Battle’s sign), as periorbital ecchymosis (raccoon sign), or by CSF rhinorrhoea or otorrhoea. Alternatively, they may be suggested by cranial nerve lesions involving the olfactory nerve (cribriform plate fracture), optic nerve (sphenoid), facial nerve (petrous) or abducens and facial nerve (sella fracture).
Skull fractures can also cause cranial nerve damage and provide an entry to the CSF for infection or air (pneumocephalus).
Examination for cerebrospinal fluid leak
Particular care must be taken to examine for CSF leaks – rhinorrhoea or otorrhoea – and signs of orbital or retromastoid haematomas (which may indicate fractures with dural tears). In these instances, meningitis is a risk and an early neurosurgical opinion should therefore be obtained. In the early stages, leakage of CSF may be obscured by haemorrhage, but any clear watery discharge from the nose is suspect and should be tested for sugar and protein. CSF, unlike a serous nasal discharge, contains sugar but little protein. However, lacrimal fluid also contains small amounts of glucose, and CSF must therefore be positively identified by protein electrophoresis and accurate measurement of the glucose.
CSF rhinorrhoea is found in about 2% of all head injuries, and in 25% of fractures of the middle third of face and nasoethmoidal complex. CSF leaks usually persist for about a week and the risk of meningitis is greatest within the first fortnight. Post-traumatic CSF leaks will usually resolve without surgical intervention. Successful management in refractory cases often involves a combination of observation, CSF diversion and/or extracranial and intracranial procedures. Occasionally, the fistula may be occluded by herniated brain but the dural tear fails to heal. If there is a dural tear, meningitis may follow after some months or years and therefore dural repair is desirable.
In all patients with ocular or orbital injuries, the orbit should be examined radiologically, usually by CT for fracture; if the latter is suspected, the patient should undergo exploration and receive prophylaxis, as recommended for penetrating intracranial wounds.
Prophylactic antimicrobials are needed if there is a meningitis risk and should therefore be given to all patients with a penetrating brain injury (PBI), where the risk of intracranial infection is high because of contaminating foreign objects, skin, hair and bone fragments driven into the brain. Antimicrobials are also indicated in compound depressed skull fractures, CSF leaks or fractures of the middle third. The infecting agents in meningitis in one study were Gram-positive cocci (Staphylococcus haemolyticus, Staphylococcus warneri, Staphylococcus cohnii, Staphylococcus epidermidis and Streptococcus pneumoniae) or Gram-negative bacilli (Escherichia coli, Klebsiella pneumoniae or Acinetobacter anitratus). Gram-positive strains were sensitive to vancomycin. All Gram-negative strains appeared resistant to ampicillin and third-generation cephalosporins, but sensitive to imipenem and to ciprofloxacin. Many bacteria causing post-traumatic meningitis are now resistant to sulphonamides. Recommended antimicrobials that readily reach the CSF and are well absorbed when given orally include co-amoxiclav, or cefuroxime with metronidazole, or azithromycin, or vancomycin and ceftazidime. Effective alternatives are rifampicin or minocycline.
Intracranial bleeding
Intracranial haematomas may be intracerebral (subarachnoid) haematomas – usually not amenable to surgical intervention; or epidural or extradural (between dura mater and skull) – usually due to tearing of the middle meningeal artery after a fracture of the temporal bone and evolving rapidly; these are neurosurgical emergencies requiring burr holes through the skull to drain the clot and ligate the bleeding vessel. The haematoma forms a tumour-like mass, which compresses part of the brain and raises ICP as it expands. Clinically, the typical story is of a heavy blow followed by loss of consciousness. There is usually then a period of apparent recovery (lucid interval), followed by signs of rising ICP. If the clot is not removed, death from respiratory arrest follows. A radiograph showing a fracture line crossing the line of the middle meningeal artery strongly suggests extradural haemorrhage and CT scanning will confirm the diagnosis.
Subdural haematomas – between the dura and leptomeninges – are venous and associated with underlying brain contusion. Acute subdural haematoma is often caused by a tear in the arachnoid and may be associated with laceration or contusion of the brain. Clinically, there is a latent interval after the injury, followed by progressive deterioration of consciousness and development of symptoms somewhat similar to those of an extradural haematoma. Once coma has developed, up to 50% die. Early operation to evacuate the clot through burr holes improves survival. Chronic subdural haematoma can be caused by a very mild injury but, nevertheless, the veins between the pia and the dura mater get torn and blood leakage into the subdural space is very slow. There is a fibroblastic response and eventually the haematoma becomes enclosed in scar tissue or, occasionally, resorbed. Clinically, the head injury, especially in an elderly person, may be so slight as to have been forgotten but, after several weeks, or even months, symptoms such as headache, dizziness, slowness of thinking, or confusion and disturbance of consciousness develop. There may be localizing signs, such as hemiparesis or aphasia; the patient may have ptosis and be unable to look upwards (pressure on the third nerve).
Neurological assessment
After head injury, approximately 50% of patients have permanent after-effects, such as paralyses, loss of speech, impaired vision, epilepsy, disturbances of personality or severe mental defects, disabling them for life. Delayed effects may result from ischaemia, hypoxia, cerebral oedema, intracranial hypertension and/or abnormalities of cerebral blood flow. Cranial nerve injuries in patients with head injuries may indicate a basal skull fracture or other lesion; cranial nerves I, II, III, V, VII and VIII are most vulnerable (Table 24.6 and Ch. 13). Sense of smell is disturbed or lost (anosmia) in 5–10% of head injuries, since the olfactory nerves are damaged in frontal bone injuries and fractures involving the ethmoid cribriform plate. CSF rhinorrhoea is often associated. Traumatic anosmia improves in only about 10% and perversion of the sense of smell may develop during recovery, effects that are remarkably troublesome or even disabling, but untreatable. The goals of head injury treatment are therefore to detect any damage and prevent or reverse secondary insults to the damaged brain, such as from hypoxaemia, hypotension and intracranial bleeding or haematoma, and to allow recovery of as much damaged brain tissue as possible.
Table 24.6
Cranial nerve lesions complicating head injuries
| Nerve lesion | Usual site of injury | Comments |
| I (olfactory) | Ethmoidal complex (may be no fracture) | Anosmia (usually permanent); apparent loss of taste |
| II (optic) | Orbita or sphenoid | Pupil dilated and unreactive to light, but consensual reflex retainedb; partial or complete blindness |
| III (oculomotor) | Orbita | Affected eye looks down and out. Pupil dilated, unreactive to light. No consensual reflex. Loss of medial and vertical movement of eye. Divergent squint |
| IV (trochlear) | Orbita | Diplopia only on looking down. Similar features result if superior oblique muscle is entrapped. Pupil reacts normally |
| V (trigeminal) | Middle fossa, orbita, maxilla or mandible | Commonly extracranially. Anaesthesia or paraesthesia in sensory area |
| VI (abducens) | Orbit |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


