CHAPTER 20 EXTRACTION IMMEDIATE IMPLANT RECONSTRUCTION
SINGLE TOOTH TO FULL MOUTH
When two-stage, root-form osseointegration implants were first introduced, the techniques for using them were based on the assumption that implants would be placed into healed alveolar ridges.1,2 In the last 12 to 15 years, however, the concept of placing both two-stage and now one-stage implants into fresh extraction sites has excited the field of implant reconstruction.3–5
Immediate implant placement offers both the patient and clinician a number of benefits (Box 20-1). Elimination of the postextraction wait for primary healing of the soft tissues and regeneration of the osseous structure shortens the overall treatment time. Even when extraction is atraumatic, the absence of a functioning dental unit causes the bone to undergo a catabolic phase that results in varying degrees of atrophy. In contrast, placing the implant immediately after extraction preserves the bony receptor site as well as the surrounding soft tissue. Another benefit of immediate placement after extraction is that design and fabrication of the prosthesis typically are improved, resulting in better-finished lines and margins, heights of contour, emergence profiles, and interproximal architecture. Finally, since the extraction socket is totally visible, the surgeon can better determine the appropriate alignment and parallelism relative to the adjacent and opposing residual dentition. The result is a better implant position, which in turn ensures better final function and aesthetics6 (Table 20-1).
 Methodology and Clinical Guidelines
Methodology and Clinical Guidelines
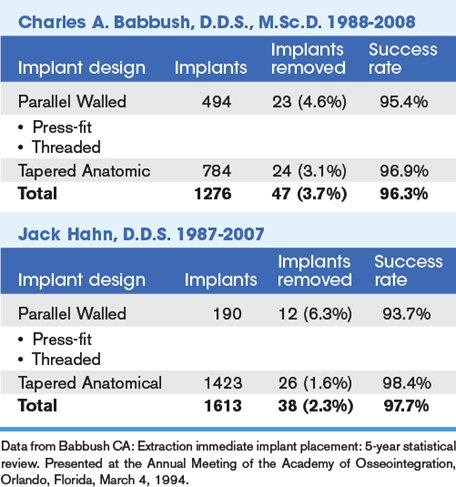
In the early 1990s only one article was available for review in evaluating this concept.3 Because of this lack of research a 5-year retrospective study was instituted by Babbush. From 1988 to 1993 the author placed 163 implants in fresh extraction sites in 80 patients. The male/female ratio among the patients was 2 to 1, and the average age was 59 years, +/- 14 years. Indications included single-tooth replacement, unilateral distal free-end, bilateral distal free-end, intermediary piers, and full-arch reconstruction in both the maxilla and mandible.6,7 Only two implants failed. Life-table statistical analysis revealed a 96.4% 5-year survival rate for this series of cases.8
Based on this experience, the following clinical surgical guidelines were developed (Box 20-2):
The procedure is typically initiated by reflecting the mucoperiosteal tissues and surgically removing the tooth as atraumatically as possible. The recent introduction of the X-Trac Extraction Systems (A. Titan Instruments, Hamburg, NY) has made it possible in many instances to atraumatically remove the tooth in toto.9 When a tooth has previously been treated with endodontic therapy, however, it may be brittle or even ankylosed to the surrounding bone. In such cases, to best preserve the osseous receptor site, the author uses a high-speed, contra-angle handpiece with a 700 XXL to section the tooth longitudinally and dissect the segments, which are then removed with the aid of periotomes.
Whenever the osseous defect exists in proximity to the implant, grafting and/or the use of a barrier membrane should be considered (Box 20-3). Grafting is also indicated when the labial or buccal bone is eggshell-thin or so thin that the implant and/or the burs can be seen through the bone or when an actual dehiscence exists. Such compromised areas are usually avascular. A bone graft will improve the vascular supply and prevent secondary dehiscence due to avascular necrosis. The use of resorbable barrier membranes may also be considered. Barrier membranes should be immobilized with fixation devices whenever possible. By following these guidelines for extraction and immediate placement, the author has achieved excellent outcomes in more than 1000 cases.
 Tapered Implants
Tapered Implants
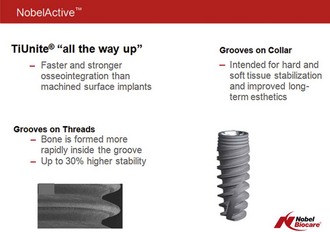
Although excellent results can be obtained when placing standard implants in fresh extraction sites, tapered anatomically shaped implants have a broad base of indications. Instead of having a uniform diameter, such implants more closely mimic the shape of the natural tooth roots (Figure 20-1). They are wider at the cervix than at the apex. Tapered implants such as the Replace Groovy and NobelActive (Nobel Biocare, Yorba Linda, CA) are available in various lengths (8, 10, 13 and 16 mm) and surface diameters 3.5, 4.3, 5 and 6 mm. The NobelActive has 10, 11.5, 13, and 15 mm lengths and 3.5, 4.3, and 5.0 mm diameters. Both systems have TiUnite (Nobel Biocare) surface properties allowing for intimate interaction between the implant surface and the surrounding living cells and tissue.10
Dental studies have shown that textured implant surfaces, including appropriately placed surface grooves on the threads of implants, can increase stability compared to implants without textured surfaces.11–14 The literature suggests that grooved implants could optimize implant stability, particularly when clinical conditions do not favor implantation. Extensive biomechanical and histological testing of oxidized titanium implants has identified the optimal groove for promoting growth and stability. Bone forms preferentially within the grooves, compared to other parts of the implant, and these implants are effective even in soft bone. Grooves are even more effective when they are used in bone of lower quality, when their enhanced osseoconductive properties produce a guiding effect on bone-forming cells.
A rabbit model study involving oxidized implant surfaces concluded that bone was stimulated to form along an implant grooved by 110 and 200 micron-wide and 70 micron-deep grooves. The 110 micron-wide groove significantly increased resistance to shear forces. Research shows that bone preferentially bonds with grooves, so grooves have been extended to the collar of the implants to increase surface area and bone-to-implant contact.15,16
 NobelActive Expands Treatment Options
NobelActive Expands Treatment Options
The unique design of NobelActive makes it an excellent choice in all indications, but especially in regions of diminished bone quantity or quality, due to its bone condensing capability, compatibility with shorter drilling protocols, and ability to change direction on insertion (Figure 20-2).
Clinical Benefits
 Bone Quality
Bone Quality
Vertical Bone Quantity
The amount of bone available for implant retention differs from site to site. The unique design features of the NobelActive implant allow it to be anchored and stabilized in as little as 3 mm of bone anywhere along the implant’s length (Figure 20-4). The thin layer of available bone can be at the implant’s apex as in a freshly extracted tooth socket or at the implant’s neck as in a sinus life situation.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses