Chapter 20
Cystic Lesions of the Jaws
Cystic lesions of the jaws are common pathologic lesions. This group of lesions comprises a number of different conditions, either odontogenic or non-odontogenic in origin.
Odontogenic cysts are the most frequent, and of these the radicular cyst is seen most often. Odontogenic cysts arise from the epithelial remnants of tooth formation, and consequently they are epithelially lined and develop in the tooth-bearing areas of the jaws. These lesions are benign, but very rare instances of associated malignancy or malignant change in the cyst wall have been reported.
Non-odontogenic cysts were classically thought to arise from epithelial remnants from the fusion of the maxillary and frontonasal processes and mandibular processes in the embryo. Aneurysmal and solitary bone cysts, on the other hand, are non-epithelial lined non-odontogenic cysts. These theories have, however, been challenged and most are now felt to be odontogenic or respiratory in origin.
Many of these lesions are slow growing and asymptomatic, often found as incidental findings at dental check-ups or with the use of panoramic radiographs for dental assessment. Accurate diagnosis and appropriate treatment are required, as these lesions will generally continue to grow and may affect adjacent teeth and other structures and even result in pathologic fracture.
The small group of developmental soft tissue cysts will be considered at the end of this chapter.
Odontogenic Cysts
Apical or Radicular Cysts
Radicular cysts are the commonest jaw cysts, comprising half to two-thirds of all such lesions. The cyst is most commonly found associated with the apex of a tooth, but lateral periodontal cysts may be found associated with lateral canals, and residual cysts persist and enlarge following extraction of the causative tooth leaving cystic remnants behind. The cyst usually arises following the development of periapical granuloma from the necrotic remnants of the dental pulp. Chronic inflammation of this tissue initially stimulates the cell rests of Malassez, resulting in epithelial proliferation. This initiation phase is then followed by a phase of cyst development, followed by cyst growth. Radicular cysts are fluid-filled lesions that expand in the jaw by osmotic pressure and cytokines cause local resorption of bone.
Radicular cysts are uncommon in children, and become more frequent in adolescents but are most often seen in adults of all age groups. They are reported to be more prevalent in men than women, although this may be due to women taking greater care of their teeth and visiting the dentist more often than men. The maxilla is more commonly involved than the mandible. Most radicular cysts present as slow-growing, painless swellings associated with a non-vital or root-treated tooth or as incidental findings on panoramic radiographs. Less frequently, radicular cysts become infected and present as a facial abscess or cellulitis.
At presentation the oral soft tissues are often normal, but careful examination may reveal a firm, hard, smooth swelling at the apex of the tooth. As the cyst enlarges the overlying bone may become resorbed leaving a soft swelling or even a thin layer of bone that may be felt to give way on palpation (egg shell crackling). As the cyst is palpated the patient may report pain. The causative tooth will be found to be non-vital and other teeth involved as the cyst enlarges may also become devitalized.
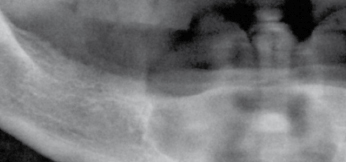
Investigation is by vitality testing of the associated teeth and periapical or panoramic radiographs. The radiographic features are of a smooth, rounded, unilocular radiolucency with a radiopaque outline associated with the apex of a non-vital tooth. Adjacent structures may be displaced by the expanding cyst (Fig. 20.1).

Treatment is by removal of the cause of the inflammation either by root canal treatment, or by extraction of the causative tooth. Small cysts are reported to regress; however, larger lesions will require enucleation. In teeth previously root treated with a good periapical seal, or those restored with a post crown where the post is large and threatens root fracture if an attempt is made to remove it, apicectomy can be performed if the tooth is not extracted.
Following enucleation, the soft tissue overlying the bony cavity is closed and the resulting hematoma ossifies. Some surgeons prefer to fill large cavities with corticocancellous bone chips to accelerate bone regeneration, but there are no studies to show that this practice has benefit. More recently the use of bone morphogenic protein has been described to improve rates of bone regeneration. In mandibular lesions where removal of the cyst threatens to cause a postoperative pathologic fracture, miniplates can be placed prior to closure to strengthen the weakened area of jaw. Patients with very large lesions and those who are severely medically compromised and unable to withstand a prolonged oral surgical procedure may be best treated by marsupialization (decompression) of the cyst allowing bony regeneration. The cyst is decompressed and the lining sutured to the oral mucosa.
Residual Cysts
Residual cysts develop from residual periapical infection or from cyst fragments left following extraction of a non-vital tooth. They present with similar features to the radicular cyst and radiographically are found as isolated, circumscribed, unilocular radiolucent lesions in the alveolar process but without an obvious causative tooth (Fig. 20.2). They require enucleation or marsupialization as described in Apical or radicular cysts.
Lateral Periodontal Cysts
These lesions are usually asymptomatic and identified radiographically between the roots of teeth, often in the mandibular canine and premolar area. The adjacent teeth are vital and the cysts are thought to arise from the cell rests within the periodontal ligament. The botyroid odontogenic cyst and glandular odontogenic cyst are variants of the lateral periodontal cyst and are both uncommon. Botyroid odontogenic cyst is found in adults of 50 years and older, and involves the bicuspid area of the mandible. The glandular odontogenic cyst may be multilocular and is reported to be prone to recurrence. Treatment is usually by enucleation, although on occasion extraction of the involved tooth may be required.
Dentigerous Cysts
Dentigerous or follicular cysts account for approximately one sixth of dental cysts. They are a fluid-filled expansion of the dental follicle and are attached to the crown of the tooth at the cemento-enamel junc/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


