2
Oral Health and Quality of Life
- Oral health-related quality of life (OHRQoL) refers to how patients’ oral health affects their ability to function (e.g., chew and speak), their psychological and social well-being, and whether they experience pain/discomfort.
- Several valid and reliable OHRQoL scales are available to assess children’s and adults’ OHRQoL.
- OHRQoL can guide clinicians to gain a better understanding of their patients’ oral health-related experiences and thus can increase the degree to which clinicians engage in patient-centered care.
- OHRQoL scales offer researchers an opportunity to assess subjects’ OHRQoL as a valuable outcome measure in basic science, clinical, and behavioral research.
- OHRQoL is a useful concept for dental educators because it focuses students on gaining a better understanding of their patients’ oral health-related experiences and care.
- A review of OHRQoL research shows that this concept can be useful in communicating oral health-related concerns to persons outside of the profession; it shows the power of adaptation and acceptance of patients who lack access to care, and it points to the need for a differentiated approach when assessing OHRQoL.
When the first edition of Behavioral Dentistry was published by Mostofsky, Forgione, and Giddon in 2006, research on oral health-related quality of life (OHRQoL) had just begun to develop. The chapter entitled “Quality of Life and Oral Health” (Inglehart, 2006) was therefore mostly an introduction to this topic, a reflection on the historical journey that led to research in this content area plus a discussion of the role of OHRQoL in oral health-related research, clinical practice, and dental education. Seven years later, extensive research activity related to OHRQoL has taken place, and the field is at a critical point: a Medline search with the term “quality of life” in November 2012 resulted in 104,667 hits overall; a search for “quality of life” together with “periodontal disease” led to 286 citations; a search for “quality of life” and “dental caries” yielded 184 references, and 192 citations were found when this term was combined with “orthodontics.” Considering this situation, this chapter has to go beyond offering an introduction to OHRQoL considerations and a discussion of their relevance for dental researchers, clinicians, and educators. It has to provide an analysis of the research conducted so far and provide a description of the current status quo of this research field. Based on the review of the oral health-related research conducted during the past decade, three conclusions will be discussed. First, the argument is made that OHRQoL can be a powerful communication tool when advocating for any kind of oral health-related services for patients, may it be related to educating patients about oral health promotion, or teachers or other professionals about considering oral health-related issues in their educational efforts, or even politicians involved in making healthcare-related decisions. Second, when considering the challenges concerning access to oral care that many patients still face on a daily basis in the United States, it is interesting to understand that OHRQoL research shows the amazing ability of humans to adapt to adverse circumstances, for example, to live with oral health-related functional impairments and/or pain/discomfort on a daily basis. This finding raises the question of what can and should be done in response. Finally, the review of the literature clearly shows that there is a need to consider OHRQoL not merely as a general construct, but to also realize the value of differentiated assessments and their impact on the way that researchers’, clinicians’, and dental educators’ professional behavior and thinking might be affected by such a differentiated approach.
Oral Health-Related Quality of Life: An Introduction
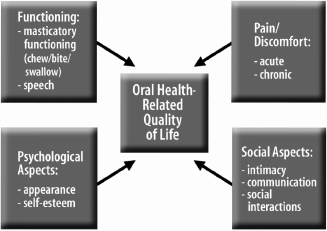
Oral health-related quality of life (OHRQoL) can be defined as assessments of how oral health affects quality of life related to (a) oral functioning (such as being able to chew, bite, swallow, or speak), (b) psychological well-being (such as a person’s satisfaction with the appearance of their teeth and smile, and self-esteem), (c) social well-being (such as the level of comfort when eating or speaking in front of others), as well as (d) pain/discomfort (Inglehart & Bagramian, 2002a) (Fig. 2.1).
Fig. 2.1. Oral health-related quality of life: an overview.
Before the term OHRQoL was introduced in the 1990s, patients’ oral health and outcomes of dental treatments were likely to be measured with objective indicators, such as patients’ functional status (e.g., number of missing teeth), and the degree to which caries (e.g., number of decayed, missing, or filled teeth or surfaces due to caries) or periodontal disease (e.g., indicators of probing depths or attachment loss) were present. The introduction of OHRQoL opened up a new perspective by suggesting considerations of how oral health/disease and the treatment of oral disease affect patients’ lives in general. It moved the perspective from being bio-dentally oriented to taking a “bio-psycho-social-dental” approach, in short, a patient-centered approach.
This paradigm shift from defining health and disease in a purely biological manner may have begun when the World Health Organization offered its programmatic definition of health as more than just physical health in the 1940s (World Health Organization, 1948). However, this perspective did not really systematically develop until the 1970s when scientists and patients alike began to consider it explicitly. In medicine, Engel (1977) introduced his now-famous biopsychosocial model of health in this time period. This model stressed a holistic approach to patient care and reflected on the value of treating patients instead of “body parts.” Around this same time, a change occurred in the way the term “quality of life” was used in the social sciences. Until the 1970s, quality of life had been largely used to describe societies. Starting in the 1970s, the term began to be used when analyzing individuals’ well-being (Campbell, 1976; Andrews & McKennell, 1980). In psychology, wellness began to be considered as a crucial aspect of a person’s life, and health psychology and positive psychology began to develop as independent areas of research around this time (Peterson, 2002).
While it took the health-oriented research community until the 1970s to start focusing on the concept of quality of life, one could argue that patients’ interactions with the healthcare system have always been affected by quality of life issues, such as suffering from pain or not being able to function. Thinking back in the history of dentistry, patients have been motivated to seek (or avoid) dental care because of quality of life issues since the beginning of dentistry. Having a toothache, being afraid of pain, or wanting dentures to enhance appearance and/or functioning are all related to patients’ quality of life and their motivation to visit or avoid dentists. First references to the relationship between oral health and quality of life can be found as early as 1978 when Giddon (1978) discussed the relationship between the mouth and patients’ quality of life (see also Giddon, 1987). However, OHRQoL was not empirically explored until the early 1990s when the National Institute of Dental and Craniofacial Research (NIDCR) introduced the concept of OHRQoL to the scientific community by funding two major conferences with a focus on this term and supporting significant numbers of research studies on this topic (Bryant & Kleinman, 2002). The first conference was organized by Slade in 1996 and focused on the measurement of OHRQoL (Slade, 1997a). Slade brought together the leading researchers on OHRQoL, such as Atchison (Atchison & Dolan, 1990), Cohen (Cohen & Jago, 1976), Gift (Gift & Redford, 1992; Gift & Atchison, 1995), Kressin (1996), Locker (1988), Reisine (1988), Sheiham, Maizels, and Maizels (1987), and Strauss (Strauss & Hunt, 1993) for a conference in Chapel Hill, NC, and collected their contributions in a book that documented the state of the art of measuring OHRQoL at that time. In May 2000, Bagramian and Inglehart organized the second NIDCR-funded conference as an interdisciplinary workshop on OHRQoL at the University of Michigan (see Inglehart & Bagramian, 2002b). This meeting had over 80 participants from as far away as Great Britain and South America who worked together with researchers from dentistry, medicine, nursing, psychology, and public health to reflect on the role of OHRQoL for clinicians, as well as basic, clinical, and behavioral researchers and dental educators in the oral health sciences. These two meetings have inspired numerous research studies since then and made the term OHRQoL widely used—as literature searches mentioned previously showed.
Having a chapter on OHRQoL in this volume on Behavioral Dentistry can show how a behavioral science concept can enrich and refocus research in the oral health sciences, how it can contribute to making clinicians more patient centered, and how it can guide dental/dental hygiene educators in their efforts to educate patient-centered and culturally sensitive future providers who see the value of working in interdisciplinary teams, including behavioral scientists.
Oral Health-Related Quality of Life: How Do We Assess It?
One major step in establishing a new concept in a scientific field is to develop reliable and valid measurement instruments. Slade (2002) provided an excellent overview of the three ways OHRQoL is assessed, namely, with social indicators, global self-ratings of OHRQoL, and multiple-item surveys of OHRQoL. Social indicators of OHRQoL, such as the days of restricted work due to dental visits, or days of work missed because of dental pain (see Reisine, 1985, for a first pioneering study; Gift, 1992), or children’s restricted activity days due to dental problems or dental visits (General Accounting Office, 2000), can serve an important function by showing that oral disease has a clear impact on society as a whole. Global self-ratings of OHRQoL usually ask respondents in surveys such as the third National Health and Nutrition Examination Survey (NHANES) of the U.S. adult population to rate their dental health on a 5-point scale ranging from 1 = “poor” to 5 = “excellent” (see Gift, Atchison, & Drury, 1998). Such a global assessment can allow comparisons between different population groups in one country, or even between countries (see, e.g., the results of the International Collaborative Study; Chen et al., 1997). However, it clearly does not reflect the complexity of OHRQoL concerns. Multiple-item surveys are the instruments of choice when patients or research subjects’ OHRQoL should be assessed. Slade (2002) offered an excellent overview of 10 OHRQoL questionnaires for adults. He showed that these surveys do not only differ in the number of dimensions of quality of life they consider, but that they also range in the number of items from merely 3 items to as much as 56 questions.
One of the most widely used instruments is the Oral Health Impact Profile (OHIP; Slade & Spencer, 1994). It consists of 49 questions concerned with the respondents’ functioning, pain, physical, psychological, and social disability, and handicap. The items are answered on 5-point rating scales. A short version of this scale, the OHIP-14, is available as well (Slade, 1997b). This short version is the most widely used instrument to assess OHRQoL. It is not only used with English-speaking respondents, but has also been translated into several other languages such as Arabic (Al-Jundi, Szentpétery, & John, 2007), Dutch (van der Meulen et al., 2008), German (John, Patrick, & Slade, 2002), Hebrew (Kushnir, Zusman, & Robinson, 2004), Sinhalese (Ekanayake & Perera, 2003), Spanish (Lopez & Baelum, 2006; Montero-Martín et al., 2009), and even Vietnamese (Gerritsen et al., 2012).
In addition to these general OHRQoL scales, condition-specific scales, such as the Xerostomia-Related Quality of Life Scale (Henson et al., 2001) or the Dentin Hypersensitivity-Related Quality of Life Scale (DHS-QoL) (Inglehart, Bagramian, & Temple, 2013a), were developed as well. An example of how such condition-specific scales are designed is provided by Inglehart et al. (2013a) who developed the DHS-QoL which consists of 24 Likert-type items with 5-point answer scales (ranging from 1 = “disagree strongly” to 5 = “agree strongly”). The selection of these 24 items was based on a focus group study with 86 adult patients with DHS in 13 focus groups. The information gathered in these focus groups was used to develop a pilot survey with 61 statements concerning how DHS affected patients’ QoL. This pilot survey was administered to 294 patients (DHS: 70%) and 219 dental students (DHS: 23%). Based on the analyses of these data, 40 statements were identified for which (a) the answers of respondents with DHS versus without DHS differed significantly, and (b) high correlations between the responses and the oral exam data were found. These statements were then used in a second survey with 316 patients (DHS: 73%) and 317 dental students (DHS: 20%) in a subsequent validation study. Based on these findings, 24 items were selected for the final DHS-QoL Scale. In addition to a total DHS-QoL score, three subscores can be computed: subscale 1 assesses pain/discomfort related to DHS (n = 8 items; Cronbach’s alpha = 0.95); subscale 2 assesses general consequences of DHS on patients’ lives (n = 8 items; Cronbach alpha = 0.93), and subscale 3 measures how DHS affects patients’ behavior (n = 8 items; Cronbach’s alpha = 0.92). Factor analytically determined construct validity, as well as external validity (assessed with correlations between the DHS scores and the number of teeth with DHS as determined in oral exams) of the total and subscales were excellent.
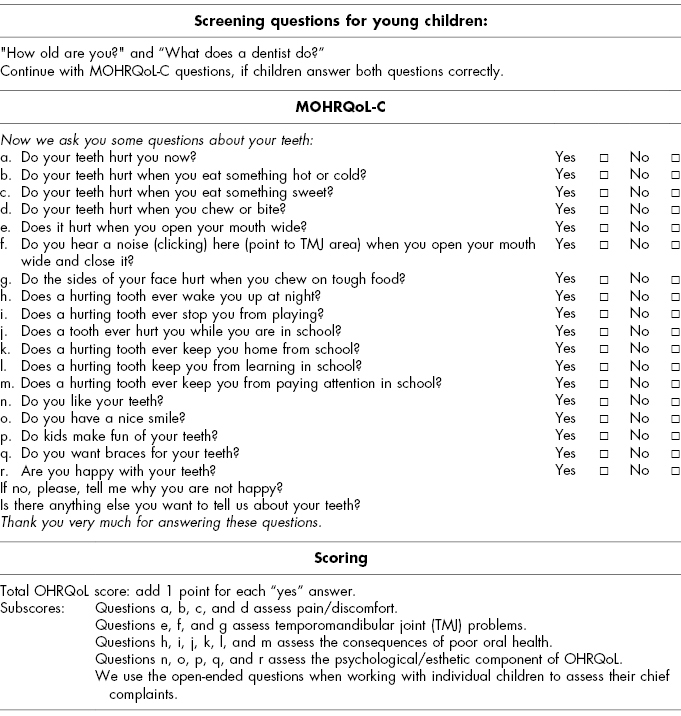
In addition to scales that assess the OHRQoL of adults, several scales have been developed to assess children’s OHRQoL. Some of these scales measure children’s OHRQoL directly by asking the children, while other scales are proxy measurements that require parents to assess their children’s OHRQoL. One scale that can be used with children as young as 5 years of age is the Michigan Oral Health-Related Quality of Life Scale—Child Version (MOHRQoL-C) (Filstrup et al., 2003; Inglehart et al., 2006). Inglehart et al. (2006) used this scale with children as young as 5 years of age. However, before administering this scale to very young children, they use two prescreening questions (“How old are you?” and “What does a dentist do?”) and then only continue to ask the MOHRQoL-C questions if the children answer both prescreening questions correctly. The scale consists of direct questions and has a “Yes”/“No” answer format (see Table 2.1 for the wording of the questions and the scoring).
Table 2.1 Michigan Oral Health-related Quality of Life Scale—Child Version (MOHRQoL-C) (Inglehart et al., 2006)
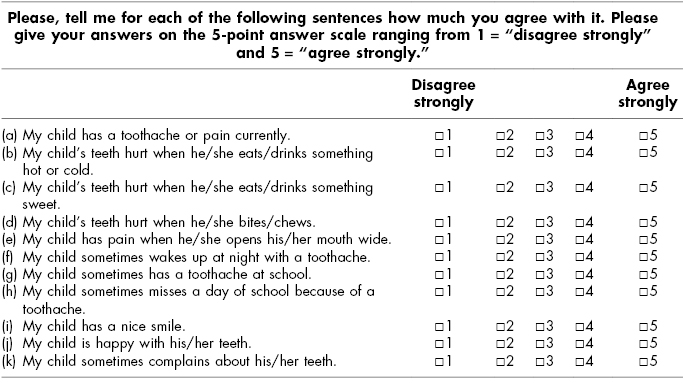
In addition to this MOHRQoL-C, the authors also developed an MOHRQoL-Parent/Proxy Version of this scale (see Table 2.2). This proxy version can be used when children are too young to answer the questions themselves or if they have special healthcare needs that do not allow them to respond to the items directly. However, such a scale has also value in itself because it allows assessing if parents are actually aware that their child has an impaired OHRQoL (see Filstrup et al., 2003). In addition, it can be quite interesting to explore whether children and parents agree on the degree to which a child’s OHRQoL and related behavior is affected by an oral health-related issue such as caries (Patel, Tootla, & Inglehart, 2007) or a cleft lip and/or palate (Munz, Edwards, & Inglehart, 2011). An additional benefit of asking parents or caregivers about another person’s OHRQoL may be that it might engage this person in reflecting on the importance of oral health for this person’s quality of life.
Table 2.2 Michigan Oral Health-Related Quality of Life Scale—Parent Version (MOHRQoL-P)
Several scales were developed to assess OHRQoL in older children. For example, Jokovic and colleagues developed the Child Perception Questionnaire (CPQ)8–10 (the subscripts 8–10 indicate the age range for which the questionnaire can be used) for assessing OHRQoL in 8- to 10-year-old children (Jokovic et al., 2004b) and the CPQ11–14 for 11- to 14-year-old children (Jokovic et al., 2002), as well as a parent proxy scale (PPQ; Jokovic et al., 2003; Jokovic, Locker, & Guyatt, 2004a). Do and Spencer (2008) showed in an evaluation study of these surveys with 1401 children between 8 and 13 years and parents that these scales had acceptable internal consistency and construct validity.
Broder and her colleagues (Broder, McGrath, & Cisneros, 2007; Broder & Wilson-Genderson, 2007; Wilson-Genderson, Broder, & Phillips, 2007) developed the Child Oral Health Impact Profile (COHIP) for children as young as 8 years of age and their caregivers. These authors found low to modest correlations between children and their parents’ proxy assessments of their children’s OHRQoL scores. Based on these findings, they argue that children’s OHRQoL should be assessed both by asking the child directly as well as collecting proxy assessments.
In summary, a review of the literature concerning measurement instruments for assessing OHRQoL in adults and in children shows that reliable and valid general scales, as well as some oral disease-specific scales, are available. This situation has allowed the inclusion of OHRQoL in a wide range of oral health-related research studies.
Oral Health-Related Quality of Life: Its Role in Research
Given the recent paradigm shift from a purely bio-dental approach to a “bio-psychosocial-dental” approach in the oral health sciences, it is not surprising that OHRQoL has begun to play an increasingly more important role in oral health-related research. Research concerning oral health issues is amazingly diverse. It ranges from basic science research, to clinical, behavioral, and public health-related studies, and it addresses quite diverse topics ranging from tissue regeneration to access to care issues. OHRQoL can play an important role in all of these different types of research.
Concerning basic science research, Somerman (2002) presented a powerful argument when she pointed out that the outcome of all research endeavors is the improvement of orocraniofacial health and ultimately quality of life, and that basic science research cannot reach this outcome in isolation. She described how basic science research has to becom/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


