Developmental Disturbances
Sadhana Shenoy, Karen Boaz, Sara Carolina Rodriguez Peña, Francisco Lopez Sanchez and Ravikiran Ongole
➧. Developmental Disorders Affecting Tongue
➧. Developmental Disorders Affecting the Lip
➧. Developmental Disorders Affecting Buccal Mucosa and Gingiva
Fordyce’s Granules (Fordyce’s Spots/Disease)
This condition is characterized by the presence of multiple discrete minute yellow colored ‘dots’, ‘spots’ or ‘granules’ involving various sites in the oral cavity such as the buccal mucosa (opposite the molar teeth), lips, oral commissures, retromolar pad, faucial pillars and the palate (Figure 1). Some authors have described the appearance as ‘rice-like’, white or yellow white papules. The sebum produced by these sebaceous glands imparts the yellow color to these spots. Each of these granules can vary in size from 1 to 3 mm. The condition is asymptomatic and usually prominent in adults and generally persist throughout life.

Figure 1 Multiple yellowish ‘dots’ on the buccal mucosa suggestive of Fordyce’s granules. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore
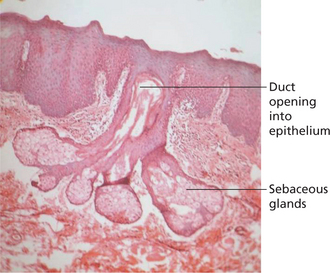
Histopathologically acinar lobules are seen below the surface epithelium. These acinar lobules usually communicate with the epithelial surface via a central duct (Figure 2). The ducts may show keratin plugging. The sebaceous cells are roughly polygonal in shape with a central nucleus. The cells contain copious amounts of foamy cytoplasm.
Lingual Tonsils
Lingual tonsils do not require any active management. The patient should be reassured and told to report any change in size or presence of symptoms. Lingual tonsillitis can be managed with antibiotics. Extensive enlargement of the lymphoid aggregates can impede intubation. Histopathological evaluation is advised when the lymphoid aggregate enlarges rapidly in size or exhibits surface ulceration.
Fissured Tongue
The fissures are seen on the dorsal surface of the tongue sometimes extending to the lateral margins. The fissures can have various morphological patterns; a single prominent groove in the midline of the tongue, multiple horizontal groves radiating from the median groove and multiple grooves in an irregular fashion (Figure 3A, B).
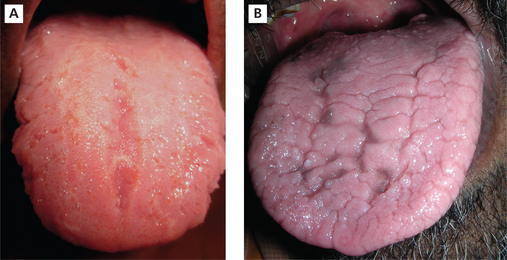
Figure 3 (A) Fissured tongue with central median groove. (B) Fissured tongue with multiple grooves in irregular fashion. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore
The tongue fissures can be seen in childhood. However, the fissures are usually prominent with advancing age. Fissured tongue is usually associated with other conditions such as geographic tongue (see Figure 21), Melkersson-Rosenthal syndrome and Down syndrome.
Leukoedema
Van Wyk (1985) studied the association between leukoedema and smoking. He examined 1996 high school students. He concluded that smoking does not cause leukoedema but may aggravate it. He also suggested that the etiology for leukoedema is multifactorial.
Clinical features
Leukoedema presents as an asymptomatic, grayish white diffuse opalescent region on the buccal mucosa and occasionally extending into the vestibule, floor of the mouth and soft palate. The surface appears spongy and usually comprises folds or grooves. It has been shown that it is more common in blacks (almost 90%) compared to whites (Figure 4).
Retrocuspid Papillae
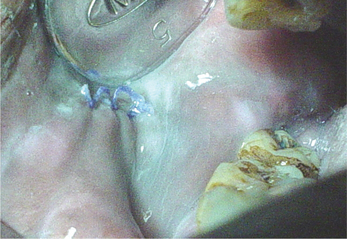
The retrocuspid papilla is a normal variation in anatomy characterized by the presence of pink colored, soft to firm, generally sessile papule or nodule (Figure 5), located on the gingiva on the lingual surface of the mandibular canines (cuspid).
D’Aoust et al (1991) studied the distribution of retrocus-pid papillae among three groups (Ecuador, Honduras and Nicaragua) of Latin American patients. He found that the retrocuspid papilla was most prevalent in children below the age of 5 years. He also found a significantly higher female predilection in the Honduras group of Latin Americans and unilateral presentation was more common. Bilateral presence of retrocuspid papillae was seen in the Nicaragua group. Retrocuspid papilla was seen involving the attached gingiva more frequently than the free marginal gingiva. Brannon et al (2003) also showed that retrocuspid papillae are common in females and young children. In the 51 cases that were evaluated, bilateral retrocuspid papillae was more common.
Histological features
Buchner et al (1990), histopathologically analyzed 30 specimens of retrocuspid papillae. They showed that almost 80% of the specimens showed loosely arranged delicate fibrous connective tissue with stellate and multinucleated fibroblasts. They also showed that significant number of specimens exhibited elongated rete ridges and/or increased vascularity.
Prominent Palatal Rugae
Palatal rugae have also been referred to as rugae palatinae and plicae palatinae transversae.
The word ruga (plural: rugae) is a Latin word meaning ridge, wrinkle or fold. For descriptive purposes palatine rugae are anatomical ridges, folds or wrinkles in the anterior part of the palatal mucosa. The rugae are present on either side of the median palatal raphe behind the incisive papilla. Approximately four to seven rugae are seen on either side of the midpalatine raphe (Figure 6).
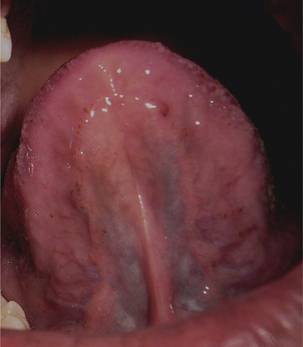
Lingual Varices
Lingual varices are characterized by the presence of tortuous dilated veins on the ventral surface of the tongue. It is estimated that approximately 10% of the patients in the 4th decade and above exhibit lingual varicosities and the extent of the varicosities increases with advancing age. Lingual varices have been referred to by various other names in literature such as phlebectasia linguae, caviar lesions and linguae varicosities.
Etiopathogenesis
Various theories have been proposed to explain the occurrence of these varices. Ettinger et al (1974) showed that the incidence of varicosities increases with age. Koscard et al (1970) reported that the elastic support to capillaries significantly diminishes with advancing age. This reduction in the elastic support of the connective tissue supporting the blood vessels leads to dilation of capillaries and formation of varicosities. It is also suggested that these are due to abnormally dilated and tortuous veins (varices), as they are not protected by surrounding tissues against hydrostatic pressure.
Clinical features
In this condition multiple, bluish-purple papular blebs are seen on the ventral and lateral borders of the tongue and occasionally seen on the lips and buccal mucosa. Ventral surface of tongue reveals the presence of tortuous and dilated veins (Figure 7). Susmita et al (2006) reported a case with palatal varicosities. These are usually seen in the elderly and are not symptomatic unless the varices are thrombosed. Jassar et al (2000) reported a symptomatic case of sublingual varices in a patient with portal hypertension secondary to liver cirrhosis.
Circumvallate Papillae or Vallate Papillae
Roughly eight to 12 large (3–5 mm in diameter) mushroom shaped papillae are arranged all along the V-shaped sulcus terminalis that divides the tongue into the body and base (Figure 8). However, occasionally they tend to grow in size when inflamed.
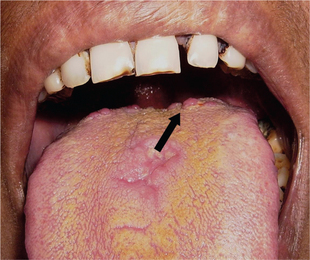
Figure 8 Mushroom-shaped circumvallate papillae. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore
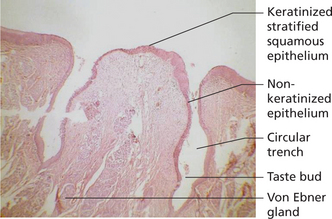
Histologically, the surface of the vallate papillae exhibits secondary papillae that are covered by stratified squamous epithelium. The epithelium lining the lateral surface of the papillae shows numerous taste buds (Figure 9). The minute ducts of the von Ebner’s glands pours its serous secretions into the base of the circular depression (trough). It is believed that the secretions of the von Ebner’s glands is the primary source of salivary lipase and it also cleanses the trough so that the taste buds can respond to various stimuli instantaneously.
Parotid Papilla
In many instances the orifice is hardly noticeable. However in some individuals a small, triangular raised pink to red color papule or nodule is readily visible. This flap of tissue covering the orifice of the Stensen’s duct is called parotid papilla (Figure 10). Parotid papillae are usually seen bilaterally. As a result of their anatomic location adjacent to the occlusal plane, the parotid papillae are common sites for formation of traumatic ulcers.
Racial Pigmentation/Physiological Pigmentation
In dark-skinned people, oral pigmentation increases, but there is no difference in the number of melanocytes between fair-skinned and dark-skinned individuals. The variation is related to the differences in the activity of melanocytes.
Clinical features
It is clinically manifested as multifocal or diffuse melanin pigmentation. The attached gingiva is the most common intraoral site of such pigmentation (Figure 11), where it appears as a bilateral, well-demarcated, ribbon-like, dark brown band that usually spares the marginal gingiva. Other sites of involvement are the tongue (Figure 12), lips, buccal and labial mucosa and perioral skin.
Hairy Tongue
This condition has also been referred to as black hairy tongue. Etiology is unknown, however certain predisposing factors include poor oral hygiene, frequent use of mouthwashes, smoking and alcohol consumption, radiation therapy for head and neck cancers, fungal infections, topical or systemic antibiotics and corticosteroids and debilitating systemic illness.
Clinical features
Though the condition has historically been referred to as black hairy tongue, the color can vary from yellow to brown to black (Figure 13). The coloration depends on the chromogenic bacteria, consumption of beverages like tea and coffee and tobacco use. This condition is usually asymptomatic. However some individuals complain of altered taste sensation, halitosis and occasionally gagging sensation.

Figure 13 LYellowish-brown colored hairy tongue. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore
Histologically hyperkeratosis of the filiform papillae is seen.
Mlandibular and Maxillary Tori
Torus/Tori
Torus palatinus
The tori in the palatal vault may vary in size from a few centimeters to larger sized lesions and are usually lobu-lated and dome shaped with a smooth surface (Figure 14). These exostoses generally tend to enlarge with age. Histopathologically smaller lesions are composed of compact bone. However larger tori may exhibit a central core of cancellous bone covered by compact bone.
Torus mandibularis
Torus mandibularis is the term used to describe exostoses occurring on the lingual surface of the mandible. It is estimated that 7–10% of the population of United States exhibit torus mandibularis. However no specific male or female predilection is reported. The mandibular tori usually occur in a symmetric fashion on the lingual surface of the mandible above the level of the mylohyoid ridge (Figure 15). The tori are usually located near the canine and premolar teeth. Occasionally the bilateral tori are so extensive that they meet at the midline. These tori are termed ‘kissing tori’.
Buccal exostoses
Buccal exostoses are benign, broad-based surface masses of the outer or facial aspect of the maxilla (Figure 16) and less commonly, the mandible (5.1:1). They begin to develop in early adulthood and may very slowly enlarge over the years.
Reactive Subpontine Exostoses
Radiographic findings
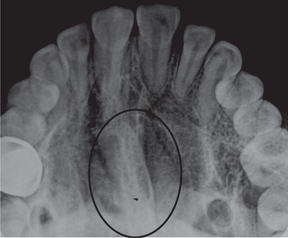
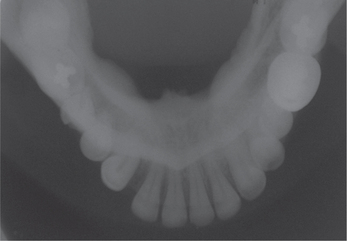
However occlusal radiographs may show a faint radiopaque shadow over the midpalatal region (Figure 17). Mandibular tori are readily visualized as radiopaque areas projecting from the lingual cortical plate on mandibular occlusal radiographs (Figure 18).
Soft Tissue Disturbances
Developmental Disorders Affecting Tongue
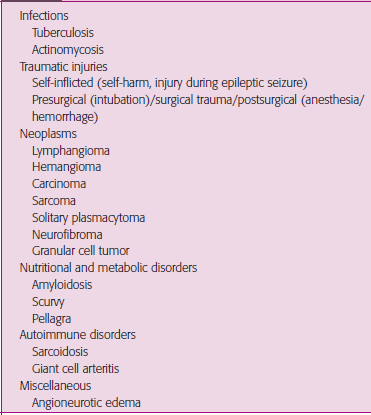
Macroglossia
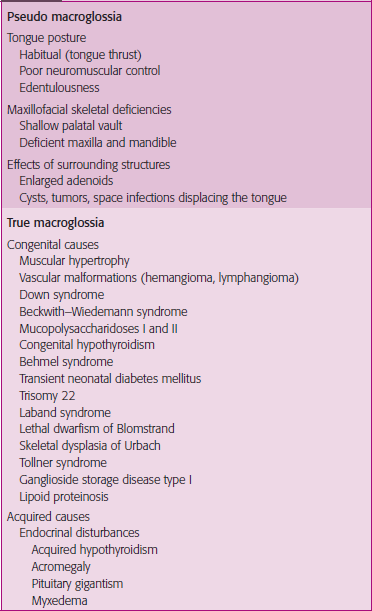
An abnormally enlarged tongue is one that protrudes beyond the teeth or the alveolar ridge in the resting position (Figure 19). Macroglossia can be broadly categorized as true macroglossia and pseudo macroglossia (Table 1). In true macroglossia enlarged tongue is associated with histological abnormalities. In pseudo macroglossia (relative macroglossia) the enlargement is apparent; though histology does not provide a pathologic explanation (e.g. Down’s syndrome).
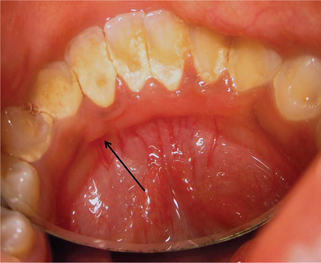
Ankyloglossia/Tongue-tie
Ankyloglossia or tongue-tie, is the result of a short, tight, thick, lingual frenulum causing tethering of the tongue tip (Figure 20). Messner (2000) reported that the incidence of ankyloglossia ranged from 0.02% to 4.8% in newborns.
Geographic Tongue
Etiopathogenesis and predisposing factors
The etiopathogenesis of the condition is still not understood. Histologically it is said to be an inflammatory condition associated with human leukocyte antigen (HLA)-DR5, HLA-DRW6, and HLA-Cw6. Eidelman et al (1976) reported that many of the parents and siblings of individuals with geographic tongue also presented with the condition. This substantiated the possibility of heredity being an etiological factor.
Marks and Simon (1979) showed a definitive association between geographic tongue and atopy.
Many authors postulate that psoriasis manifests orally as geographic tongue. Gonzaga (1996) in his investigations showed a significant association of Cw6 with both psoriasis and benign migratory glossitis. This antigen was found in 59.1% of the patients with psoriasis and 43.8% of the patients with benign migratory glossitis. Zargari (2006) in a study including 306 patients with psoriasis concluded that geographic tongue is more common in early onset psoriasis and may be an indicator of the severity of psoriasis.
Clinical features
Geographic tongue is commonly seen in the 2nd decade of life.
The appearance of the lesion typically mimics geographic outlines on a map, hence the name geographic tongue (Figure 21). It appears as circinate irregular erythematous patches which represent the atrophic filiform papillae, bound by keratotic white bands or lines which represent the regenerating filiform papillae (Figure 22).

Figure 22 Geographic tongue on the dorsum of the tongue. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore
Though this condition is typically seen involving the tongue, it can occur on other sites in the oral mucosa. Some authors use terms such as ectopic geographic tongue, geographic stomatitis, erythema migrans, erythema areata migrans, and stomatitis areata to refer to such a finding. The common ectopic sites include the buccal mucosa, labial mucosa (Figure 23), gingiva, floor of mouth and less commonly the soft palate and uvula.
Histopathologic features
Biopsy specimens should ideally be obtained from a site which includes the keratotic serpiginous margin and the atrophic area. On histopathological examination hyperkeratosis, acanthosis and slender, elongated rete pegs are seen. Neutrophil infiltrations are seen in the thick layer of keratin and to a lesser degree in other portions of the epithelium. These infiltrations produce microabscess (Munro’s abscess) in the keratin and spinous layers.
Management
All patients of geographic tongue need to be reassured of the harmless nature of the condition. In symptomatic patients palliative therapy with topical or systemic antihistaminics have proved beneficial due to their local anesthetic effect (Sigal et al, 1992). Presence of associated fissured tongue with superimposed candidal infection can be effectively managed with topical clotrimazole. Benzydamine hydrochloride mouthrinse can be used to manage burning sensation. Gibson et al (1990) in their study showed that zinc supplements proved effective for managing geographic tongue.
Lingual Thyroid
The lingual thyroid is seen as a nodular mass in the midline about 2–3 cm in diameter with a smooth surface. It appears erythematous when highly vascular. Depending on the size, it may produce symptoms of pain, feeling of fullness in the throat, dysphagia, dysphonia and dyspnea.
Developmental Disorders Affecting the Lip
Commissural Lip Pits
These small mucosal invaginations occur at the corners of the mouth on the vermillion border (unilaterally or bilaterally), possibly due to failure of fusion of embryonal maxillary and mandibular processes (Figure 25). Though considered congenital, these often develop later in life – prevalence in children (0.2–0.7%) being much lower than in adults (12–20%). Males are more often affected than females. An autosomal dominant pattern of transmission is noted in some families. In most cases, they are asymptomatic and are discovered on routine examination; they may express saliva on squeezing. The depth of these pits range from 1mm to 4 mm. Associated preauricular pits may be seen in some. They are generally not associated with facial or palatal clefts. Histopathologically they are similar to paramedian lip pits.
Double Lip
Here a mucosal fold appears on the mucosal side of the lip, commonly the upper lip. The congenital form is due to persistence of sulcus between the pars glabrosa and pars villosa of the lip. The acquired form may be due to trauma, repeated sucking on the lip or as part of Ascher’s syndrome (double lip, blepharochalasis and non-toxic thyroid enlargement). In most cases, it becomes visible only when the lip is tense or while smiling. Histopathologically normal structures are seen with a slight abundance of minor salivary glands. Excision is the treatment for esthetic reasons.
Cleft Lip and Cleft Palate
Cleft lip results from failure of merging of epithelial groove between the medial and lateral nasal process by penetration of mesodermal cells. Cleft palate is the result of epithelial breakdown with in growth failure of mesodermal tissue and lack of lateral palatal segment fusion. Most cleft cases are polygenic but the 5% of cleft cases associated with syndromes are said to be monogenic (Tables 2 and 3). Environmental factors like nutritional deficiencies, stress, infections, alcohol, drugs, toxins and ischemia may cause clefts.
Table 2
Syndromes associated with cleft lip
Achondroplasia
Beckwith–Wiedemann syndrome
Fetal alcohol syndrome
Goldenhar syndrome
Gorlin syndrome
Treacher Collins syndrome
Van der Woude syndrome
Waardenburg syndrome
Table 3
Syndromes associated with cleft palate
Achondroplasia
Beckwith–Wiedemann syndrome
Cleidocranial dysplasia
Crouzon syndrome (craniofacial dysostosis)
Ehlers–Danlos syndrome
Fetal alcohol syndrome
Gorlin syndrome (basal cell nevus syndrome)
Marfan syndrome
Pierre Robin syndrome
Rubinstein–Taybi syndrome
Treacher Collins syndrome (mandibulofacial dysostosis)
Van der Woude syndrome
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses