19 FRAMEWORK DESIGN AND METAL SELECTION FOR METAL-CERAMIC RESTORATIONS
Tooth-colored restorative materials have evolved from the soluble silicate cements of the past to the composite resin materials and resin-modified glass ionomer cements of today. Currently, metal-ceramic prostheses are widely accepted and are the most commonly used extracoronal restoration.1,2 They combine the superior fit of a casting with the outstanding esthetics of dental porcelain. Because the ceramic veneer is chemically bonded to the metal substructure, this restoration is not subject to the discoloration problems associated with acrylic resin veneer crowns and, when appropriate clinical and laboratory protocols are followed, excellent longevity can be predicted.3 In addition, the material properties of dental porcelain are better able than resin to withstand wear under functional loading.
The concept of combining a brittle material with an elastic material to arrive at more desirable physical properties has many engineering applications. Dental porcelains (which are, chemically speaking, glasses) resist compressive loading but tend to succumb to tensile stress. Therefore, the metal substructure must be designed so that any tensile stresses in the porcelain are minimized.
Restorations with porcelain occlusal surfaces must be planned carefully. Although they are esthetically very acceptable, these restorations have disadvantages, especially wear of the opposing enamel.4 Ideally, an esthetic restoration should wear at approximately the same rate as the enamel it replaces (about 10 μm per year5). In addition, the restoration should not increase the wear rate of an opposing enamel surface. Dental porcelain is more abrasive of enamel than of other restorative materials (e.g., gold or amalgam6–10) and has been implicated in severe occlusal wear, particularly when the porcelain is not glazed or highly polished (Fig. 19-1).11 This factor should be considered whenever a metal-ceramic restoration is being designed,12 and the practitioner should realize that although abrasiveness may be correlated with the composition of the ceramic material, the selection of a lower fusing ceramic (sometimes labeled by the manufacturer as “low-wear”) does not necessarily mean less enamel wear.13 Less wear on opposing teeth was cited as the most important need for improvement of posterior tooth-colored crowns.1 In addition, porcelain occlusal coverage leads to restorations with lower strength,14 and anatomically correct occlusal form with sharp cusps can be difficult to obtain in dental porcelain.

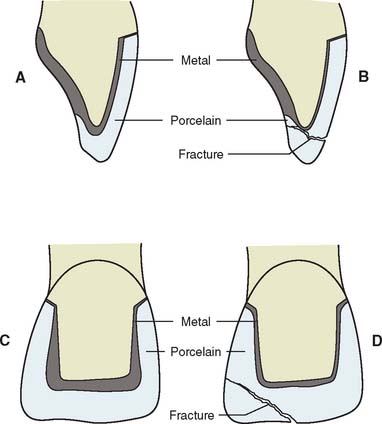
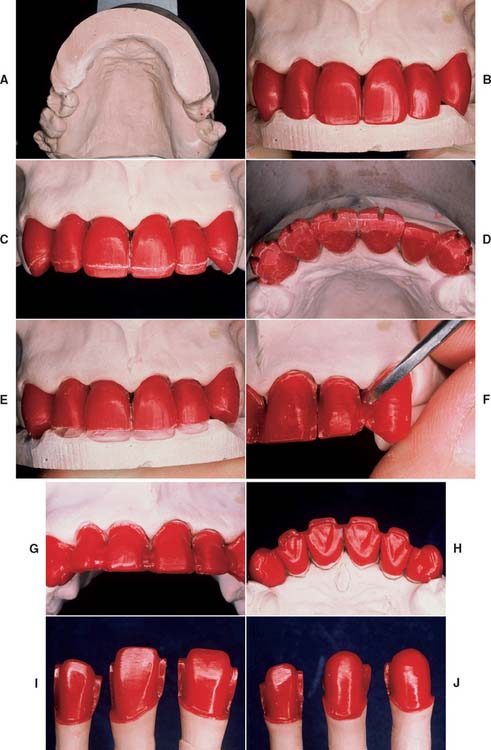
Fig. 19-1 A to D, Destructive enamel wear associated with metal-ceramic restorations.
(Courtesy of Dr. M. T. Padilla.)
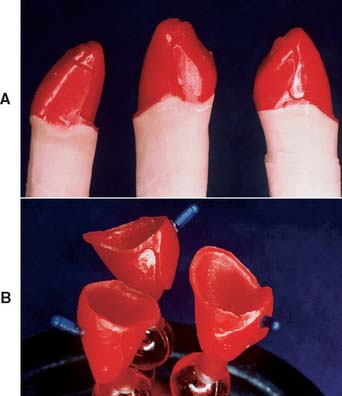
Some technicians may attempt to fabricate a framework by dipping the die into molten wax, obtaining an even thickness. After the excess wax is trimmed away, a gingival collar is added, and the pattern is sprued, invested, and cast. When this is completed, the veneer is then applied. This technique almost always produces an uneven porcelain thickness, with an increased potential for material fracture as a result of the porcelain’s lack of proper support (Fig. 19-2). If porcelain thickness is not well controlled, appearance suffers as well, because the shade of the final crown depends on porcelain thickness.15 For predictable success, the framework must be carefully designed and shaped.
PREREQUISITES
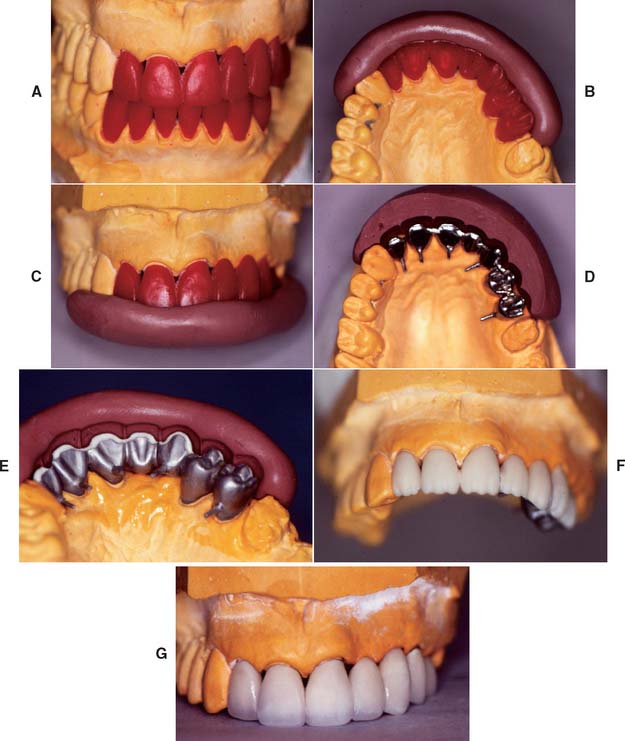
The framework design for a fixed prosthesis should be considered during the treatment planning stage (see Chapter 3) and should be evaluated at the diagnostic tooth preparation and waxing stages, particularly in more complex treatments. A properly designed framework for a metal-ceramic crown or fixed dental prosthesis (FDP) can be achieved routinely only by waxing the restoration to complete anatomic contour first and then cutting back a consistent amount for the veneer. This allows an even thickness of porcelain, proper porcelain-metal interfaces, good connector design, and optimally placed occlusal contacts.
Waxing to Anatomic Contour
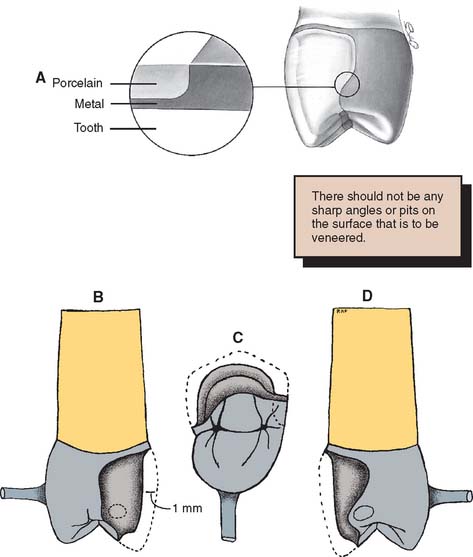
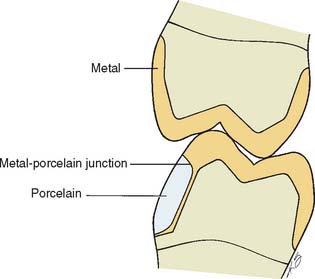
The main objective in waxing a framework is a substructure that supports a relatively even thickness of porcelain. Simultaneously, if the retainer is to serve as part of an FDP, it must allow for proper connector configuration and location. Furthermore, the restoration must conform to the normal anatomic configuration of the tooth that is being replaced. At the porcelain-metal interface, the ceramic material should be at least 0.5 mm thick. The framework should be shaped to allow for a distinct margin so that the porcelain is not overextended (Fig. 19-3). There should be no abrupt contour change between the metal and the adjacent porcelain.
The most effective way to consistently meet these criteria, with a minimum number of failures, is to develop the final contours of the proposed restoration in wax (Fig. 19-4). Once completed, the area to be veneered can be demarcated and an even thickness of wax removed. If this technique is not followed, one or more of the objectives is almost certainly missed, and the contours of the framework are not in harmony with the required ceramic configuration (Fig. 19-5).
Occlusal Analysis
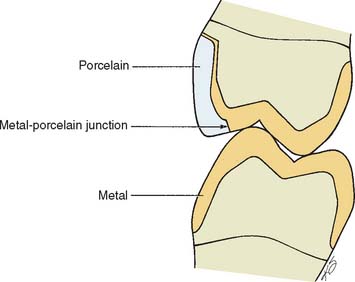
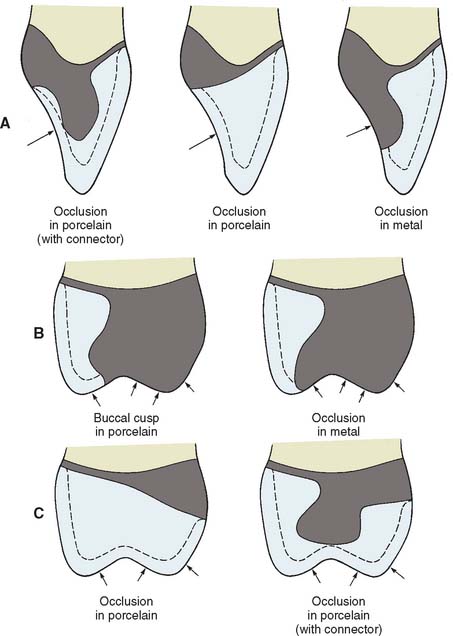
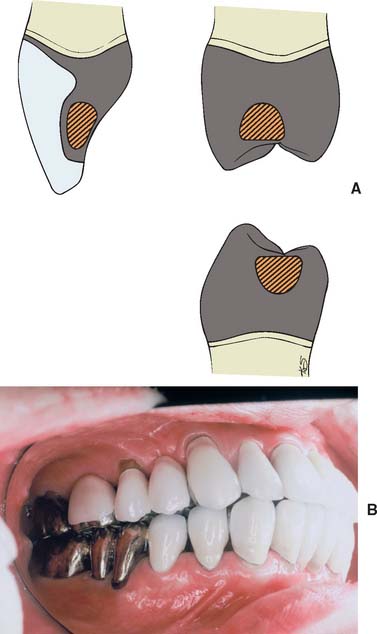
The centric stops of any metal-ceramic restoration can be located on either porcelain or metal. However, they must be at least 1.5 mm away from the junction16 to prevent porcelain fracture from deformation of the metal (Fig. 19-6). Care is needed to minimize sliding contacts over the porcelain-metal interface. When this is not possible, the framework must be modified so that the porcelain is well supported in the area of functional contact.
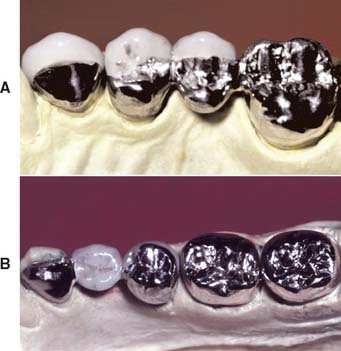
Existing restorations in the opposing arch can influence framework design. Because sliding contact of a porcelain restoration with a cast crown abrades the gold, the framework design must be modified as necessary. A complete cast crown in the mandibular arch presents little difficulty. It can be opposed by a maxillary restoration with only a metal occlusal surface and a facial ceramic veneer (Fig. 19-7). An existing metal crown on a maxillary molar, however, restricts the design of a mandibular metal-ceramic restoration if metal-to-porcelain contact is to be avoided (Fig. 19-8). Here the facial veneer can no longer be extended to include the buccal cusp tips and associated centric stops without contacting the opposing restoration. A complete cast crown is usually preferred because most patients do not show the facial surfaces of their mandibular posterior teeth. In other situations, particularly on mandibular first premolars, a facial veneer is esthetically essential, and the design of opposing restorations should allow for it (Fig. 19-9).
CUTTING BACK
The criteria for waxing to anatomic contour are discussed in Chapter 18. This section deals with cutting back the veneering area.
Step-by-Step Procedure
Designing the cut-back
Esthetic and functional needs govern the design of the veneering surface. The ceramic veneer should extend far enough interproximally, particularly in the cervical half of the restoration, to avoid metal display. Wherever possible, the functional occlusal surfaces should be designed in metal, because an accurate occlusion is then easier to achieve (Fig. 19-10). However, esthetic demands may require extension of the porcelain veneer (e.g., on the mesial incline of a mandibular buccal cusp). The extent to which a restoration can be veneered is determined largely by the location of the centric stops.
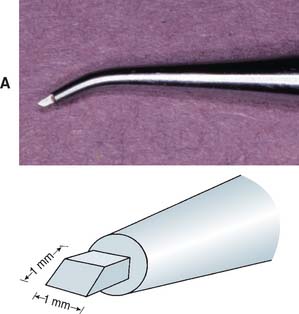
Troughing the pattern
Finishing
Connector design
Pontics
Evaluation
Immediately before the investing stage, the following criteria should have been met:
METAL SELECTION
Clinicians and dental laboratories face a potentially bewildering set of choices when selecting alloys for metal-ceramic restorations. Both noble metal and base metal casting alloys exist, and there are different alloy types for each of these two major groups. There are advantages and disadvantages for each alloy type, including significant differences in cost. Successful clinical practice depends on the selection of a compatible metal-porcelain combination that provides predictable results, depending on the particular patient’s case. Improper selection can cause catastrophic failure (Fig. 19-16). For a better understanding of the different properties provided on the packaging of casting alloys, the meanings and clinical relevance of these properties are discussed next.
Dental Connotations of Mechanical and Physical Properties for Ceramic Alloys
Modulus of elasticity
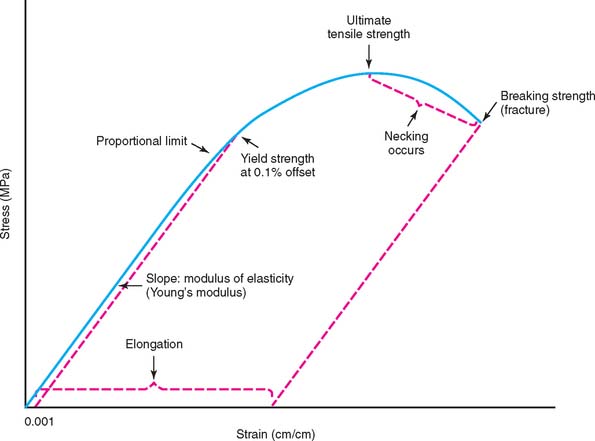
Figure 19-17 illustrates schematically the tensile stress-strain plot for a ductile casting alloy that undergoes substantial permanent deformation before fracture. This plot consists of two portions: (1) a linear or elastic region that ends at the proportional limit, where the stress is proportional to strain, and (2) a subsequent curved region corresponding to plastic or permanent deformation (which terminates when the test specimen fractures). The modulus of elasticity (also called Young’s modulus) is the slope of the stress-strain plot in the elastic region. The elastic modulus has the same value for tensile and compressive strains, which occur during bending of a prosthesis, in which regions on opposite sides of the neutral axis (centerline for a symmetric cross section) undergo opposite senses of deformation. An alloy with a higher modulus of elasticity has greater stiffness or rigidity for elastic deformation. For the fabrication of a long-span FDP, an alloy with a relatively high modulus of elasticity to reduce the amount of bending deflection under loading is preferred, because excessive flexure can cause fracture of the brittle porcelain (Fig. 19-18). The modulus of elasticity has units of stress/strain and is reported for dental alloys in units of gigapascals (1 GPa = 109 Pa = 145,000 psi [pounds per square inch]). The unit of 1 Pa = 1 N/m2 is much too small to be useful for the elastic modulus of materials.
Proportional limit and yield strength
In standard testing practice, the proportional limit of an alloy is determined by placing a straight edge on the stress-strain plot (or performing this operation with computer software) and noting the value at which the plot first deviates from a straight line. The proportional limit is often considered synonymous with the elastic limit, which corresponds to the value of stress at which permanent deformation occurs. However, the value of the elastic limit is highly dependent on the sensitivity of the strain-measuring apparatus. Moreover, precise location of the proportional limit on the stress-strain plot is somewhat problematic. Consequently, dental alloy manufacturers generally report the yield strength (sometimes called offset yield strength), which corresponds to the amount of stress for a very small designated amount of permanent deformation, at 0.1% or 0.2% (permanent strains of 0.001 or 0.002, respectively). The unit for yield strength is megapascal: 1 MPa = 106 Pa = 145 psi. As shown in Figure 19-17, the yield strength is obtained by constructing a line parallel to the initial straight-line portion of the stress-strain plot, starting with the specified value of offset on the horizontal strain axis and then noting the point of intersection with the curved portion of the plot. Because the 0.2% yield strength can be substantially higher than the 0.1% yield strength for a given alloy, depending on the rate of work hardening (slope of the curved portion of the stress-strain plot), manufacturers specify the offset value at which the yield strength was determined on the alloy packaging. The yield strength is often called the useful strength of a dental alloy, because stresses caused by biting forces should not exceed the yield strength and result in permanent deformation of the alloy. Although a sufficiently high value of yield strength is essential for a ceramic alloy, values that are too high create difficulties when the casting is adjusted in the dental laboratory or dental office.
Hardness
The Vickers hardness number (VHN) is generally measured for dental alloys by means of a symmetric diamond pyramidal indenter. The VHN is the quotient of the indenting load and the surface area of the indentation, for which the square of the mean diagonal length is multiplied by a constant related to the indenter geometry. The Knoop hardness number (KHN), obtained with a diamond indenter having long and short axes, is sometimes reported for dental alloys. For the KHN, only the length of the long diagonal of an indentation is measured, and the indenting load is divided by the unrecovered projected area of the indentation. Harder alloys, which have smaller indentations, have higher VHN and KHN values. Conversion scales available for the two different hardness tests should be used with caution, because such conversions are alloy dependent. Both the VHN and KHN are measures of the microhardness, in contrast to the older Brinell and Rockwell tests, in which much larger indenters are used to measure the macrohardness. When measuring the Vickers hardness of an alloy, an understanding of the microstructure is crucial. Use of the large indenting load of 1 kg stipulated in standards for dental alloys provides information about the overall hardness of the alloy microstructure, whereas light indenting loads (e.g., 10 g) can be used to obtain information about the hardness of individual grains, constituents, or phases. The hardness is an important practical property, inasmuch as very high values of hardness cause difficulty in the dental laboratory when the casting is ready to be finished. Alloys with VHN or KHN values exceeding that of enamel (approximately 350) cause abrasive wear of opposing teeth.
Ultimate tensile strength
The UTS (also called tensile strength or simply strength) is the maximum point on the stress-strain curve (see Fig. 19-17) and represents the greatest value of stress that can be developed in the alloy without fracture. The unit of measure for UTS is megapascal. Two types of stress-strain curves are observed for tensile testing of casting alloys. Alloys of high ductility undergo substantial necking between the UTS and the breaking strength, as shown in Figure 19-17. Other alloys of more limited ductility undergo much less necking, and the stress continues to increase after the yield strength until fracture occurs at the UTS. The UTS has minimal practical importance for a ceramic alloy, because the corresponding permanent strain does not occur under clinical conditions for a restoration. Nevertheless, />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses