Provisional Restorations
Chapter Objectives
On completion of this chapter, the student will be able to:
1. State the purpose of provisional coverage.
2. List examples of circumstances that may require provisional coverage.
3. Identify the criteria necessary for a high-quality provisional restoration.
4. List the properties of provisional materials.
6. Distinguish between intracoronal and extracoronal restorations.
7. List the advantages and disadvantages of pre-formed and custom crowns.
8. Differentiate between direct and indirect fabrication techniques.
9. List the advantages and disadvantages of acrylic and composite provisional materials.
11. List patient education and home care instructions.
12. Fabricate and cement a metal provisional crown.
13. Fabricate and cement a polycarbonate crown.
Key Terms defined within the chapter
Indirect Fabrication provisional restorations made on a cast outside the patient’s mouth
Intracoronal Restoration a restoration within the crown of the tooth, such as an inlay
Direct Fabrication provisional restorations made directly inside the patient’s mouth
The increased demand for retention of natural teeth and new technology in restoring and replacing tooth structure have increased the need for high-quality fixed prosthodontic, pedodontic, and endodontic procedures. Fabricating provisional coverage is an important aspect of these treatments. Once the tooth has been prepared, the exposed dentin must be protected from the thermal, chemical, mechanical, and bacterial effects of the oral environment. Adjacent tissues must be protected, and the position of the tooth must be maintained. All of this must be accomplished with provisional coverage, with additional considerations of esthetics, function, and patient comfort.
The dental assistant and the dental hygienist may be called on to fabricate, repair, remove, or maintain, and give home care instructions for, the provisional restoration for various periods of time during which temporary coverage is necessary.
Dental Procedures that may Require Provisional Coverage
Provisional coverage may be required in general, pedodontic, endodontic, and prosthodontic cases. Whenever a situation arises wherein a permanent restorative material cannot be placed at the time of preparation, a temporary or provisional material may be chosen (Table 17-1).
TABLE 17-1
Dental Procedures Requiring Provisional Coverage
| Procedure | Type of Provisional Coverage |
| Endodontic access preparation | Closes endodontic access preparations between appointments |
| Vitality of the tooth is in question | Allows the pulp to respond to therapeutic agents or to recover from the trauma of preparation |
| Emergency care | Prevents additional damage and improves esthetics and function while awaiting a permanent solution |
| Awaiting permanent restoration | Allows time for laboratory fabrication of cast and porcelain restorations |
| Restoration of implants | For long-term provisional coverage while the implant site is allowed to heal |
| Restoration of primary teeth | Placed on primary teeth because of extensive caries, pulpotomies, or pulpectomies until permanent teeth erupt |
The patient wears this provisional coverage to protect the tooth for a short period of time, generally 2 weeks to a month. In cases involving complex treatments such as implants and complex prosthodontic procedures, a longer time may be required.
Criteria for Provisional Coverage
Criteria for a properly placed provisional restoration include maintenance of tooth position, protection of hard and soft oral structures, and establishment of function and esthetics. If these criteria are not met, pulpal and periodontal irritation, tooth migration, and patient dissatisfaction will very likely occur.
Maintain Prepared Tooth Position to Adjacent and Opposing Teeth
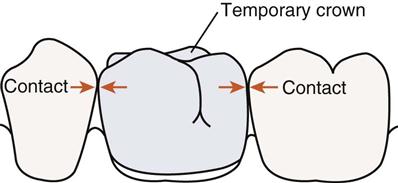
When a tooth has been prepared to receive a crown, sufficient tooth material has been removed to create a space between the adjacent tooth and the opposing teeth. A prepared tooth without occlusal/incisal and proximal contact may migrate laterally or occlusally/incisally within a few days. The restoration, which was designed to fit the tooth in its original position, may now be too high because of occlusal/incisal migration or may not seat properly as a result of lateral migration of the prepared tooth. If the provisional restoration itself is too high, the results may be those associated with trauma from occlusion, and if it does not contact adjacent teeth, gingival irritation from food impaction is likely. It is important that precise occlusal/incisal and proximal contacts be provided for. The provisional restoration should share the forces of adjacent and opposing teeth.
Protect the Exposed Tooth Surfaces and Margins
When the tooth is prepared, the dentinal tubules are exposed to potentially harmful thermal, chemical, mechanical, and bacterial effects of the oral cavity. These opened tubules leave the pulp vulnerable to the effects of temperature and of chemical irritants of the material placed. Provisional materials placed near the pulp must have no adverse chemical effect and must be sufficiently insulating to protect the pulp from thermal assaults.
The margins, or finish line, of the preparation are particularly susceptible to fracture if not adequately supported. Well-adapted provisional restorations protect the finish line from fracture and from marginal leakage of oral fluids and bacteria. If the finish line is damaged, the permanent restoration will no longer fit precisely, leaving space for future leakage of oral fluids. The process of caries may even begin during the time the provisional restoration is in place. Because temporary luting agents are highly soluble and may wash out from under the provisional restoration, they cannot be expected to make up for marginal deficiencies.
Protect the Gingival Tissues
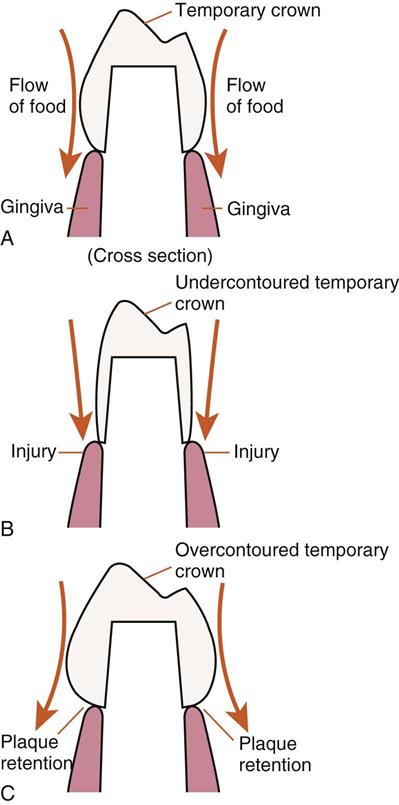
Most crown preparations extend subgingivally, making the margins and the overall contour of the provisional restoration critical to periodontal health. Periodontal tissues are susceptible to irritation from overcontoured, overextended, or overhanging margins; trauma from food impaction; and buildup of plaque. Margins must be flush with the preparation. If a margin is overextended, the resultant tissue irritation may lead to gingival recession, adversely affecting the cosmetic effect of the permanent restoration. All surfaces of the provisional restoration must be properly contoured and must maintain contact with adjacent teeth. If surfaces are undercontoured or contacts weak or nonexistent, the process of chewing will excessively force food directly onto the gingiva rather than deflecting it facially and lingually. An overcontoured restoration may trap plaque by not allowing for any self-cleansing or gingival stimulation from the chewing process. Both scenarios may lead to irritation, inflammation, and recession (Figure 17-1).
Provide Function and Esthetics
The provisional restoration should restore ideal occlusal/incisal and surface anatomy. As was previously mentioned, deficiencies in contour or contact of the provisional restoration may lead to problems that compromise or prevent the ideal placement of a permanent restoration. Patients must be able to chew, speak, and clean the provisional restoration as they would function with a permanent one. In addition, it is important to consider the importance of esthetics in collaboration with concerns for function. Provisional restorations must look like natural tooth structures whenever esthetics is important. Matching shades and customizing provisional materials to duplicate the natural teeth will greatly enhance patient acceptance and thus the success of the provisional restoration (Figure 17-2).
Properties of Provisional Materials
Materials used to fabricate provisional restorations must have properties that comply with the specific requirement of the situation and area in which they are placed. Although most provisional restorations are in place for up to 2 to 3 weeks, provisional coverage may be required for extended periods of time. Strength and hardness are important for posterior and extracoronal restorations. Tissue conditions in many areas will not impede the construction of provisional restorations with the direct technique. However, when conditions warrant, the compatibility of tissues and the chemical reaction during fabrication must be a consideration. Esthetic concerns are important for many applications; provisional restorations are no exception. In addition, considerations of handling are of special concern in areas difficult to access.
Strength
Materials must have sufficient compressive and tensile strength to resist the forces of mastication. Materials that are used for temporary bridges must also have sufficient flexural strength to resist deformation from flexing during mastication. Brittle materials such as composite resins do not hold up well when used for long span bridges or with patients who are bruxers.
Hardness
Surface hardness must be sufficient to resist abrasion and wear for the period through which the provisional restoration is to be worn. The material should also be able to be polished to a smooth surface and should retain that surface throughout its use.
Tissue Compatibility
The material should not produce any additional irritation to pulpal or gingival tissues during or after setting reactions. Materials that have adverse setting reactions must be carefully considered and may be more appropriate if the indirect fabrication technique is used. In addition, for patient comfort, materials should not absorb or give off odors or taste.
Esthetics
Materials used in areas of esthetic concern must match tooth structures and must have good color stability and stain resistance.
Handling
Materials must be fast and easy to use, reliable, and inexpensive. The material should have sufficient working time and simplified technique to allow for fabrication. For many customized provisional materials, the working time must also allow for removal from the mouth while still elastic for trimming before reinsertion. For these materials, tear strength, that is, the ability of the material to resist tearing or distortion on removal from the mouth or model, is a consideration. The setting time must be fast and must accommodate difficult to access areas when light-activated materials are used. Materials should be repairable to account for defects and to modify fit. Adding provisional material directly to the margins for repair will help provide good marginal integrity, and relining the provisional with a new mix of material will ensure a good fit. Materials must be economical to use; provisional coverage must not be excessive in terms of cost of materials or time of fabrication.
Provisional Materials
The choice of provisional material is generally dependent on type of preparation, area of the mouth, and operator preference. Provisional materials include metals, polycarbonate, acrylics, composites, and cements. These materials may be used alone or in combination, such as an aluminum shell crown lined with acrylic. Provisional restorations may be pre-formed (e.g., stainless steel or polycarbonate crowns) or made specifically for individual procedures (e.g., custom acrylic or composite crowns and intracoronal restorations).
Provisional cements, acrylic, or composite materials are mixed and placed in a plastic state and allowed to harden directly in the preparation or on a stone model. Cements are limited to intracoronal placement; provisional acrylic and composites can be used for extracoronal coverage as well.
Pre-formed crowns have the advantage of convenience, in that they are already pre-made in a variety of sizes and anatomic forms. This saves time because it eliminates the need for a crown template and is particularly useful in emergency situations and for badly broken-down teeth. Even though they come in different sizes, time must be spent establishing contact, contour, occlusion, and marginal integrity.
Customized crowns are more versatile and more consistently meet the criteria for successful provisional restorations. They do, however, require the additional step of obtaining a template or matrix for the final product. This template is a reproduction of the tooth structures as they exist before the preparation. This additional step can be further complicated if the original tooth is badly broken down or fractured.
Temporary luting cements are used to cement provisional crowns in place.
Pre-formed/Prefabricated Crowns
The process of temporization using pre-formed crowns includes the use of stainless steel and aluminum crowns, polycarbonate, and celluloid crown forms lined with acrylic or composite materials (Figure 17-3). The pre-formed crown will become the outer surface of the provisional crown, and an acrylic or composite material or strong cement will occupy the inner portion of the crown. As was previously mentioned, this method may be time saving, particularly in emergency situations when the patient has a fractured tooth, but does not consistently produce successful temporization when less than ideal situations exist. A crown with exact interproximal and length dimensions may require considerable adjustment of the pre-formed crown. Because the prepared tooth is much smaller than this pre-formed shell, a reline of acrylic or composite material is generally required. Metal crowns are generally used only in posterior cases, with polycarbonate and celluloid forms used on anterior teeth. Pre-formed crowns may be used for single crowns only and are not appropriate for temporary bridges.
Stainless Steel Crowns
The stainless steel crown is the most durable of the pre-formed crowns, providing provisional coverage lasting months and even years (Figure 17-4). The stainless steel crown has been used traditionally to restore primary teeth. These durable and economical restorations are now being considered for older adults, in cases where financial and health concerns would otherwise result in the recommendation of extractions. The primary advantage of these crowns is their malleability, which provides for good contact, occlusion, and marginal integrity. The crown is cut with crown and bridge scissors and is crimped and contoured at the contact and margins with crimping and contouring pliers. If the stainless steel crown is replacing the use of a cast restoration for prolonged periods of time, minimal reduction of the tooth is ideal to preserve natural strength and protect the pulp. With the marginal seal and occlusion intact, these crowns may be a solution to long-term provisional coverage of posterior teeth. Margins of stainless steel crowns are never a replacement for cast restorations.
Aluminum Shell Crowns
Aluminum shell crowns are used for provisional coverage of posterior teeth. Lined with acrylics or composites and cemented with temporary cement, a well-fitted aluminum shell crown can last for several weeks. The softness of the metal allows for easy manipulation of the contact, occlusion, and margins, because the metal can be stretched and burnished without wrinkling. These crowns are easily trimmed with crown and bridge scissors to adjust their length. Because of their softness, these crowns wear easily and must be checked for occlusal integrity.
Polycarbonate, Polymer, and Celluloid Crown Forms
Pre-formed polycarbonate crowns, similar to their metal partners, come in several sizes and shapes. Unlike metal, they are rigid and may have to be adapted with acrylic burs and disks or may be carefully cut with sharp crown scissors. The primary advantage is their esthetics for replacement of anterior teeth and their compatibility with acrylic resins to further customize the fit and margins.
Pre-formed celluloid forms and polymer crowns are filled with acrylic resins or composites, which are matched to tooth shade, and then are inserted onto the prepared tooth in much the same way that a template is used in the direct fabrication technique. The form must first be cut to fit the tooth; this can be accomplished easily with scissors. Usually one or two small holes are placed in the occlusal portion of the crown form to allow excess resin or composite material to flow out when the crown form is seated. This prevents trapping air and creation of voids in the material.
Customized Provisionals
The use of acrylics and composites, both self-cured and light-cured, to produce high-quality custom provisio/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses