Treatment of Chronic Mandibular Hypomobility and Growth Disorders
“ALTHOUGH RARE, NEVER FORGET THE OTHER POSSIBILITIES.”
—JPO
The preceding two chapters addressed the most common categories of temporomandibular disorders (TMDs) observed in the general practice of dentistry. This chapter deals with the remaining two categories, chronic mandibular hypomobility and growth disorders. Although these disorders occur less frequently than the others, it is equally important that they be appropriately identified and managed with proper definitive and supportive therapy.
Chronic Mandibular Hypomobility
The predominant feature of this disorder is the patient’s inability to open the mouth to a normal range. Chronic mandibular hypomobility is rarely accompanied by painful symptoms or progressive destructive changes. Therefore the decision to initiate treatment should be carefully considered. When mandibular movement is so restricted that function is significantly impaired, treatment is indicated. When pain is associated with chronic hypomobility, it usually originates from an inflammatory reaction secondary to movement beyond the patient’s restriction. This may occur as a result of either the patient’s attempt to open beyond the restriction or extrinsic trauma that forces the mandible beyond the restriction. When inflammatory symptoms are present, treatment is indicated to resolve the inflammation. However, when a patient presents with chronic mandibular hypomobility and is still able to function normally without pain, the best therapy is often no treatment. Supportive therapy may sometimes be helpful, but definitive therapy is often contraindicated.
Chronic mandibular hypomobility is subdivided into three categories according to etiology: ankylosis, muscle contracture, and coronoid impedance.
Ankylosis
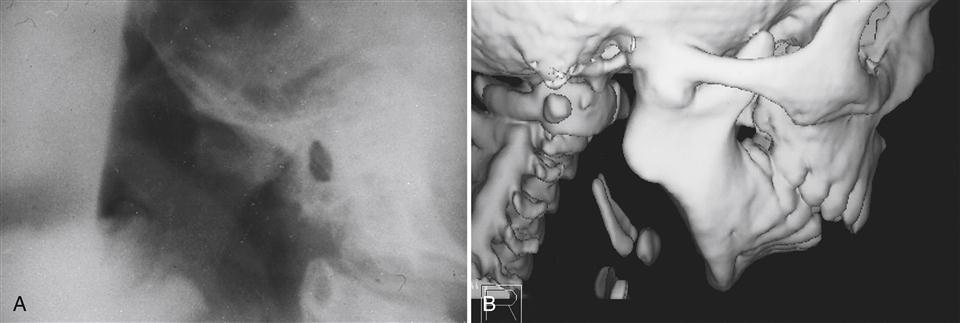
Ankylosis by definition means abnormal immobility of a joint. The two basic types of ankyloses are differentiated by the tissues that limit the mobility: fibrous and bony. A fibrous ankylosis is most common and can occur between the condyle and the disc or the disc and the fossa. A bony ankylosis of the temporomandibular joint (TMJ) would occur between the condyle and fossa; therefore the disc would have to have been absent from the discal space prior to the ankylosis. Bony ankyloses are rare and represent a more chronic and extensive disorder (Figure 14-1). Since the etiology and treatment of fibrous and bony ankyloses are similar, they are discussed together.
Etiology
The most common etiology of ankylosis is hemarthrosis (bleeding within the joint) secondary to macrotrauma.1–4 Fibrous ankylosis represents a continued progression of joint adhesions (Chapter 13) that gradually creates a significant limitation in joint movement. Chronic inflammation aggravates the disorder, leading to the development of more fibrous tissue. When bony structures become involved, bony ankylosis is more likely.
History
Patients report limited mouth opening without any pain. The patient is aware that this condition has been present for a long time and may not even feel that it poses a significant problem.
Clinical characteristics
In many cases of ankylosis the condyle can still rotate, suggesting adhesions in the superior joint space. When this occurs, movement may still be possible in the inferior joint space between the condyle and the inferior surface of the disc. Therefore the patient may be able to open approximately 25 mm interincisally. The clinical examination discloses a relatively normal range of lateral motion to the affected side but restricted movement to the unaffected side (Figure 14-2). During mouth opening, the opening pathway deflects to the ipsilateral side. No condylar movement is felt or visualized on radiography. When the ankylosis is bony, it can often be visualized on a radiograph or cone beam CT.
Definitive treatment
Since the patient generally has some movement (though restricted), definitive treatment may not be indicated. If function is inadequate or the restriction is intolerable, surgery is the only definitive treatment.5 Arthroscopic surgery is the least aggressive surgical procedure and therefore should be considered. Unfortunately many ankylosed joints are too attached to be freed with arthroscopy and other surgical procedures must be considered.2,4,6–11 When surgical therapy is indicated, the elevator muscles are likely to be in a state of myostatic contraction and must be appropriately treated after the ankylosis is resolved.
Supportive therapy
Since ankylosis is normally asymptomatic, generally no supportive therapy is indicated. However, if the mandible is forced beyond its restriction (e.g., by trauma), injury to the tissues can occur. If pain and inflammation result, supportive therapy is indicated and consists of voluntarily restricting movement to within painless limits. Analgesics, along with deep heat therapy, can also be used.
Capsular fibrosis
Another cause of mandibular hypomobility related to fibrotic changes is capsular fibrosis. The capsular ligament that surrounds the temporomandibular joint is partly responsible for limiting the normal range of joint motion. If the ligament becomes fibrotic, its tissues can tighten or be restricted and the movement of the condyle within the joint is also restricted, creating a condition of chronic mandibular hypomobility. Capsular fibrosis is usually the result of inflammation, which can be secondary to inflammation of the adjacent tissues but is more commonly caused by trauma. The trauma may be an extrinsic force (e.g., a blow to the face), a surgical procedure, or an intrinsic force associated with abuse of the jaw.
Definitive treatment
Because of two considerations, definitive treatment for capsular fibrosis is almost always contraindicated. First, capsular fibrosis usually restricts only the outer range of mandibular motion and is not a major functional problem for the patient.
Second, because the changes are fibrotic, therapy falls within the surgical range. However, surgery is one of the etiologic factors that can create this disorder. Therefore a surgical procedure to free the fibrous restrictions must be carefully weighed in view of the fact that it could lead to further fibrosis upon healing.
When restriction is a functional problem, physical therapy may be attempted. Ultrasound to the tissues can provide deep heat, which may help loosen the tissues. This therapy immediately followed by manual movement (distraction) of the joint may help to provide more mobility. This type of therapy is relatively innocuous and therefore may be tried. Acute hypomobilities respond better than the more chronic ones.
Supportive therapy
Since capsular fibrosis is normally asymptomatic, no supportive therapy is indicated. On occasion, when the mandible is forced beyond the capsular restriction (i.e., trauma), symptoms can begin. These are often related to the inflammatory reaction of the traumatized tissues. When this condition exists, the patient is treated with the same supportive therapy as for capsulitis.
Muscle Contracture
The definition of contracture is the painless shortening of the functional length of a muscle. There are two distinct types of contracture: myostatic and myofibrotic. Contracture of the elevator muscles can produce chronic mandibular hypomobility.
Myostatic contracture
Etiology
Myostatic contracture results when a muscle is kept from fully lengthening (stretching) for a prolonged time. The restriction may be the result of a painful condition that limits the full functional lengthening of the muscle. Therefore myostatic contracture is often secondary to another disorder. It is thought that full lengthening of a muscle is important in maintaining its functional length. During full lengthening, the Golgi tendon organs are stimulated and reflexly relate this input back to the muscle spindles establishing the functional length of the muscle. Some have suggested that the act of yawning is important in maintaining proper elevator muscle length.
If the mandible is fractured and must be wired together with the maxilla for 6 to 8 weeks, the elevator muscles cannot fully lengthen. This is a common source of a myostatic contracture of the elevator muscles. Once the fracture has healed and the wires are removed, the mouth will not immediately open to its normal 40+ mm. Instead, it may only open to about 15 to 20 mm. However, if the patient gently assists in the opening movement, a normal range of motion can gradually be achieved. This results from passive stretching or lengthening the muscle. When the muscle is physically lengthened, the Golgi tendon organs are stimulated and the feedback to the muscle spindle is to allow more lengthening. This is known as the inverse stretch reflex and is present in all musculoskeletal systems (Chapter 2). This technique is the basis for definitive treatment of myostatic contracture and is described in greater detail below.
Another clinical condition that can lead to a myostatic contracture arises when a patient wears an anterior positioning appliance continuously. Such an appliance will not allow full lengthening of the inferolateral pterygoid muscle. Therefore a myostatic contracture can develop that prevents the condyle from immediately returning to the musculoskeletally stable position. When this occurs and the patient removes the appliance, the posterior teeth will not occlude (a posterior open bite). This was a common adverse effect when anterior positioning appliances were used 24 hours per day. However, when these appliances are used only part time, as suggested in this text, the muscle has the opportunity to fully lengthen and posterior open bites are rarely observed.
History
The patient reports a long history of restricted jaw movement that may have begun secondary to a pain condition which has now resolved.
Clinical characteristics
Myostatic contracture is characterized by painless limitation of mouth opening or other jaw movements, depending on the involved muscle.
Definitive treatment
It is important that the original etiologic factor which created the myostatic contracture be identified. If this condition still exists, it must be eliminated before effective treatment of the contracture can result. Once the original cause has been eliminated, definitive treatment is directed toward the gradual lengthening of the involved muscles. This lengthening is an attempt to reestablish the original resting length of the muscles and must be done slowly over many days or weeks. If pain is elicited, protective co-contraction can result and the treatment will fail. The resting length of the muscles can be reestablished by two types of exercises: passive stretching and resistant opening.
Passive stretching
Passive stretching of the elevator muscles is accomplished when the patient opens to the full limit of motion and then gently stretches beyond the restriction. The stretching should be gentle and momentary so as not to traumatize the muscle tissues and initiate pain or an inflammatory reaction.12,13 Sometimes it is possible to assist the stretching by placing the fingers between the anterior teeth and initiating the stretch as the patient relaxes (Figure 14-3). This momentary stretch will excite the Golgi tendon organ reflexly, making the muscle spindle relax the muscle. Care should be taken not to overstretch the muscle. These passive stretching exercises are performed five or six times throughout the day. Each set should consist of a stretch that is held for 1 to 2 s and repeated four times. The stretching should not be so forceful as to produce pain. Too much force can create an inflammatory reaction in the tissues being stretched, which will compromise the outcome. The results of these exercises will not be seen immediately but only in days and sometimes even weeks. The patient must be told that this process may take some time and be encouraged to persist.
Resistant opening exercises
Resistant opening exercises take advantage of the neurologic reflex system to aid in relaxation of the elevator muscles. The mandibular elevators and depressors function according to reciprocal inhibition. In other words, to elevate the mandible, the elevator muscles must be contracted at the same time and to the same length as the depressor muscles are relaxed. The neurologic stretch reflex helps control this activity. When local muscle soreness is present in one of the muscle groups, full lengthening of the muscle becomes difficult. Neurologic feedback can be used to help achieve relaxation. This is accomplished by initiating mild contraction of the antagonistic muscle groups. When the elevator muscles will not properly relax, contraction of the depressors, provided by resistance to opening, feeds neurologic input to the elevator muscles, telling them to relax. This has been referred to as reflex relaxation.14
Resistant opening exercises are accomplished by instructing the patient to place the fingers under the chin. Opening is then attempted against the resistance (Figure 14-4). Resistant opening exercises consist of 10 repetitions repeated two or three times per day. The resistant force provided by the fingers is gentle and should not induce painful symptoms. Passive stretching of the elevator muscles is done both before and after each set of resistance exercises. When lateral restrictions are present, lateral resistant exercises can also be used in a similar manner but are less often indicated (Figure 14-5).
When passive and resistant exercises are properly employed for a patient with mandibular hypomobility, no painful symptoms result. Any pain that does develop is normally associated with an inflammatory reaction in the tissues. Pain therefore implies too much too soon and should tell the patient and therapist to decrease the force and sometimes the number of repetitions being used. Effective treatment may take weeks and should not be rushed.
Supportive therapy
Since definitive treatment should not create symptoms, supportive therapy is of little use in the treatment of myostatic contracture or, for that matter, any chronic mandibular hypomobility. When symptoms do occur, analgesics can be helpful and should accompany a decrease in the intensity of the exercise program. Thermotherapy and ultrasound can also be helpful.
Myofibrotic contracture
Etiology
Myofibrotic contracture occurs as a result of excessive tissue adhesions within the muscle or its sheaths. These fibrotic adhesions prevent the muscle fibers from sliding over themselves, thus preventing full lengthening of the muscle. Common etiologies of myofibrotic contracture are myositis or trauma to the muscle tissues.
History
The history for myofibrotic contracture reveals a previous muscle injury or a long-term restriction in the range of motion. There is no pain. Sometimes the patient will not even be aware of the limited range of opening because it has been present for so long.
Clinical character/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses