chapter 13
Temporomandibular Joint Pains
Masticatory pain that emanates from the temporomandibular joints (TMJs) is called masticatory arthralgia (Fig 13-1). Arthralgic pains can arise only from pain-sensitive structures of the joint and its ligaments. Normally, the pressure-bearing articular surfaces as well as the articular disc are noninnervated and therefore are incapable of initiating sensory response of any kind, including nociception. Proprioceptive input needed for functional guidance does not come from the articular surfaces but from proprioceptors located in the ligaments and muscles. Pain from the TMJs can therefore emanate from the associated soft tissue structures of the joint or the osseous tissues themselves. Pain emanating from the osseous structures usually only occurs after loss of the fibrous articular surface of the joint. When this occurs, it is commonly referred to as osteoarthritis. Not all joint pains, however are osteoarthritis. When the soft tissues of the joint produce pain, the condition is classified according to the tissues involved (eg, retrodiscitis, capsulitis).
Behavior of TMJ Pains
Pains that emanate from the structures of the TMJ are of the deep somatic category. As such, they display the clinical characteristics of deep somatic pain. Additionally, they are of the musculoskeletal type and therefore display the features that identify such pains, namely (1) the pain is intimately related to masticatory function, and (2) the degree of pain is proportionate to the amount of function or manual palpation.
It should be noted that most arthralgia is related to functional abuse and trauma, which may be accompanied by inflammation. Thus, arthralgia frequently displays clinical characteristics of inflammatory pain that are influenced by the location, degree, and phase of inflammation present. Such pains exhibit features that depend on local provocation and functional manipulation, as well as on the extent and confinement of inflammatory exudate. As long as joint pain occurs intermittently, it remains diffusely localized to the joint region and does not initiate secondary central excitatory effects. If arthralgia becomes continuous, however, a variety of secondary effects may become evident, such as referred pain that may be felt as headache, secondary hyperalgesia expressed as areas of deep palpable tenderness, and co-contraction activity in the masticatory musculature.
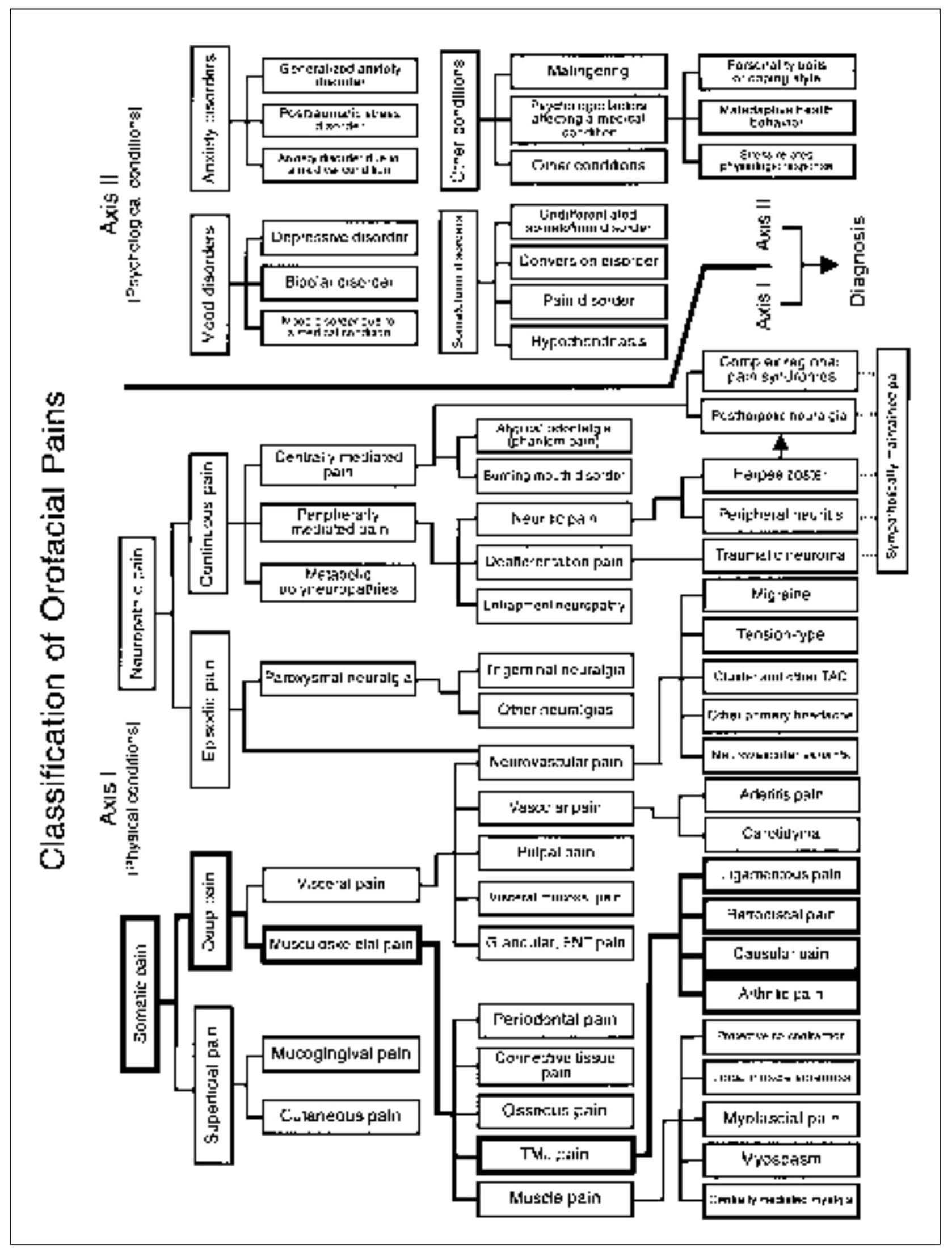
Fig 13-1 Pain classification chart highlighted to show the relationship of TMJ pains to other orofacial pain disorders.
Normal Anatomy and Function of the TMJ
The TMJ represents the articulation of the mandible to the temporal bone of the cranium (Figs 13-2a and 13-2b). The bony components of the joint are separated by a structure composed of dense fibrous connective tissue, called the articular disc. Like any mobile joint, the integrity and limitations of the joint are maintained by ligaments. Ligaments are composed of collagenous fibers that have specific lengths. As in all mobile joints, ligaments do not actively participate in the function of the joint. Ligaments act as guide wires to restrict certain movements (border movements) while allowing other movements (functional movements). If joint movements consistently function against ligaments, the length of the ligaments can become altered. Ligaments have a poor ability to stretch; therefore, when this occurs, they often permanently elongate. This elongation creates a change in joint biomechanics and can lead to certain clinical changes that will be discussed later.
The TMJ is capable of both hinging and gliding movements and therefore is known as a ginglymoarthrodial joint. For a simplified understanding of the mechanics of this extremely complex joint, let us separate it into two distinct joints. The lower joint is made up of the condyle and disc, which are attached to each other by ligaments. This combined structure is referred to as the condyle-disc complex. The condyle-disc complex allows rotational movement between the disc and the condyle. The upper joint is formed by the articulation of the condyle-disc complex with the glenoid fossa. It is between these structures that translation occurs as the condyle-disc complex moves out of the fossa during opening.
Careful examination of the condyle and disc reveals that the disc is attached to the condyle both medially and laterally by the discal collateral ligaments (Fig 13-3). These ligaments allow rotation of the disc across the articular surface of the condyle in an anterior and posterior direction while restricting medial and lateral movements. The range of anterior and posterior rotation of the disc is also restricted by ligaments. The inferior retrodiscal lamina limits anterior rotation of the disc on the condyle, whereas the anterior capsular ligament limits posterior rotation of the disc (see Fig 13-2b).
The morphology of the disc is extremely important. It is thinnest in the intermediate zone, thicker in the anterior border, and thickest in the posterior border. The condyle articulates on the intermediate zone of the disc and is maintained in this position by constant interarticular pressure provided by the elevator muscles (masseter, temporalis, and medial pterygoid). Although the pressure between the condyle, disc, and fossa can vary according to the activity of the elevator muscles, some pressure is always maintained to prevent separation of the articular surfaces. If contact between the articular surfaces is lost, a condition of dislocation exists (dislocation means separation of the articular surfaces).
Posterior to the disc are the retrodiscal tissues. These tissues are highly vascularized and well innervated. Anterior to the condyle-disc complex are the superior and inferior lateral pterygoid muscles. The inferior pterygoid muscle inserts on the neck of the condyle, whereas the superior lateral pterygoid muscle inserts on both the neck of the condyle and the articular disc. Although the inferior lateral pterygoid is active with the depressing muscles (mouth opening), the superior lateral pterygoid muscle has been shown to be active in conjunction with the elevator muscles (mouth closing).1,2 The superior lateral pterygoid muscle appears to be a stabilizing muscle for the condyle-disc complex, especially during unilateral chewing.3
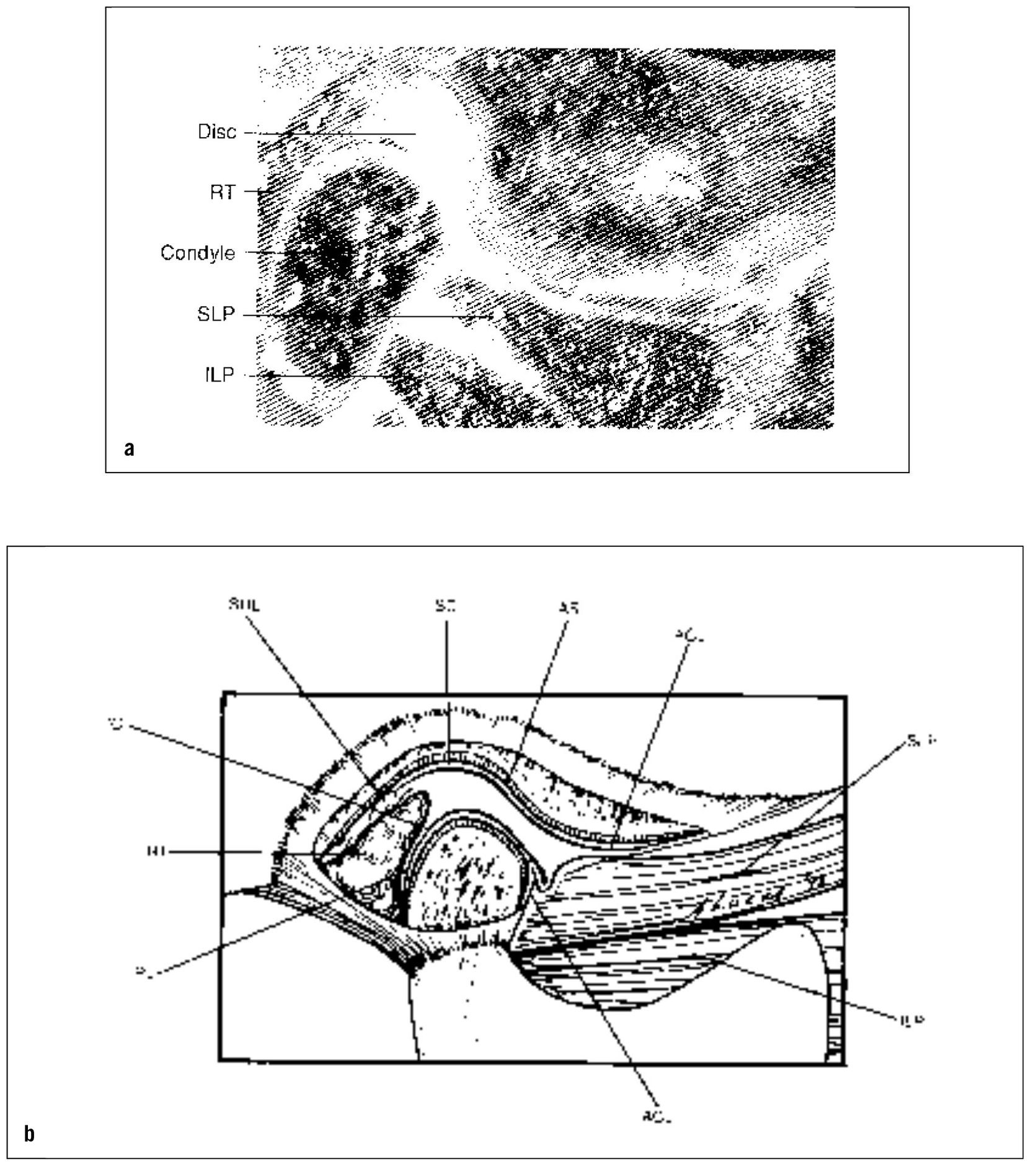
Fig 13-2 The TMJ. (a) Lateral view; (b) diagram showing the anatomic components. RT = retrodiscal tissues; SLP and ILP = superior and inferior lateral pterygoid muscles; SRL = superior retrodiscal lamina (elastic); SC and IC = superior and inferior joint cavities; AS = articular surface; ACL = anterior capsular ligament (collagenous); IRL = inferior retrodiscal lamina (collagenous). The discal (collateral) ligaments have not been drawn. (From Okeson JP. Management of Temporomandibular Disorders and Occlusion, ed 5. St Louis: Mosby-Year Book, 2003:10. Used with permission.)
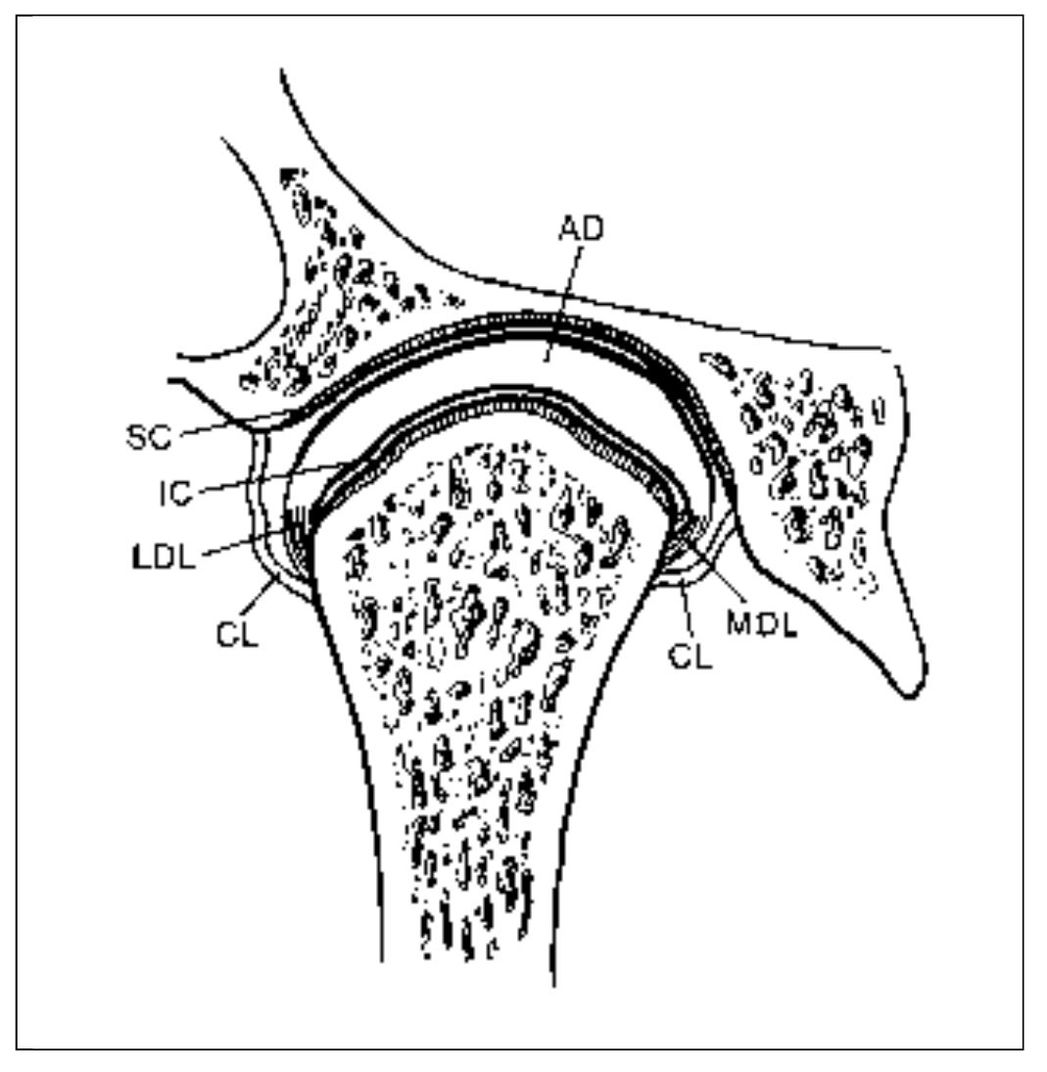
Fig 13-3 The TMJ (anterior view). The following are identified: AD = articular disc; CL = capsular ligament; IC = inferior joint cavity; LDL = lateral discal ligament; MDL = medial discal ligament; SC = superior joint cavity. (From Okeson JP. Management of Temporomandibular Disorders and Occlusion, ed 5. St Louis: Mosby-Year Book, 2003:14. Used with permission.)
When the condyle-disc complex translates down the articular eminence (mouth opening), the disc rotates posteriorly on the condyle (Fig 13-4). The superior surface of the retrodiscal tissues is unlike any other structure in the joint. The superior retrodiscal lamina is composed of loose connective tissue and elastin fibers that allow the condyle-disc complex to translate forward without damage to the retrodiscal tissues. In the closed mouth position, the superior retrodiscal tissues are passive and have very little influence on disc position. During full mouth opening, however, the superior retrodiscal lamina is fully stretched and produces a posterior, retractive force on the disc. It is important to remember that this is the only structure in the TMJ capable of providing a retractive force on the articular disc.
During opening and closing, the disc and condyle move together, not because of ligamentous attachments, but because of two fundamental features: the morphology of the disc and interarticular pressure (pressure between the articular surfaces). Because some degree of interarticular pressure is always present, the condyle maintains itself on the thinnest intermediate zone of the disc. The thicker anterior and posterior borders of the disc force it to translate with the condyle during mouth opening and closing. It is the disc’s morphology, therefore, that requires it to move with the condyle. If there is an alteration in interarticular pressure or a change in the morphology of the disc, condyle-disc movement can be altered. This, in fact, begins the biomechanical changes associated with many intracapsular symptoms.
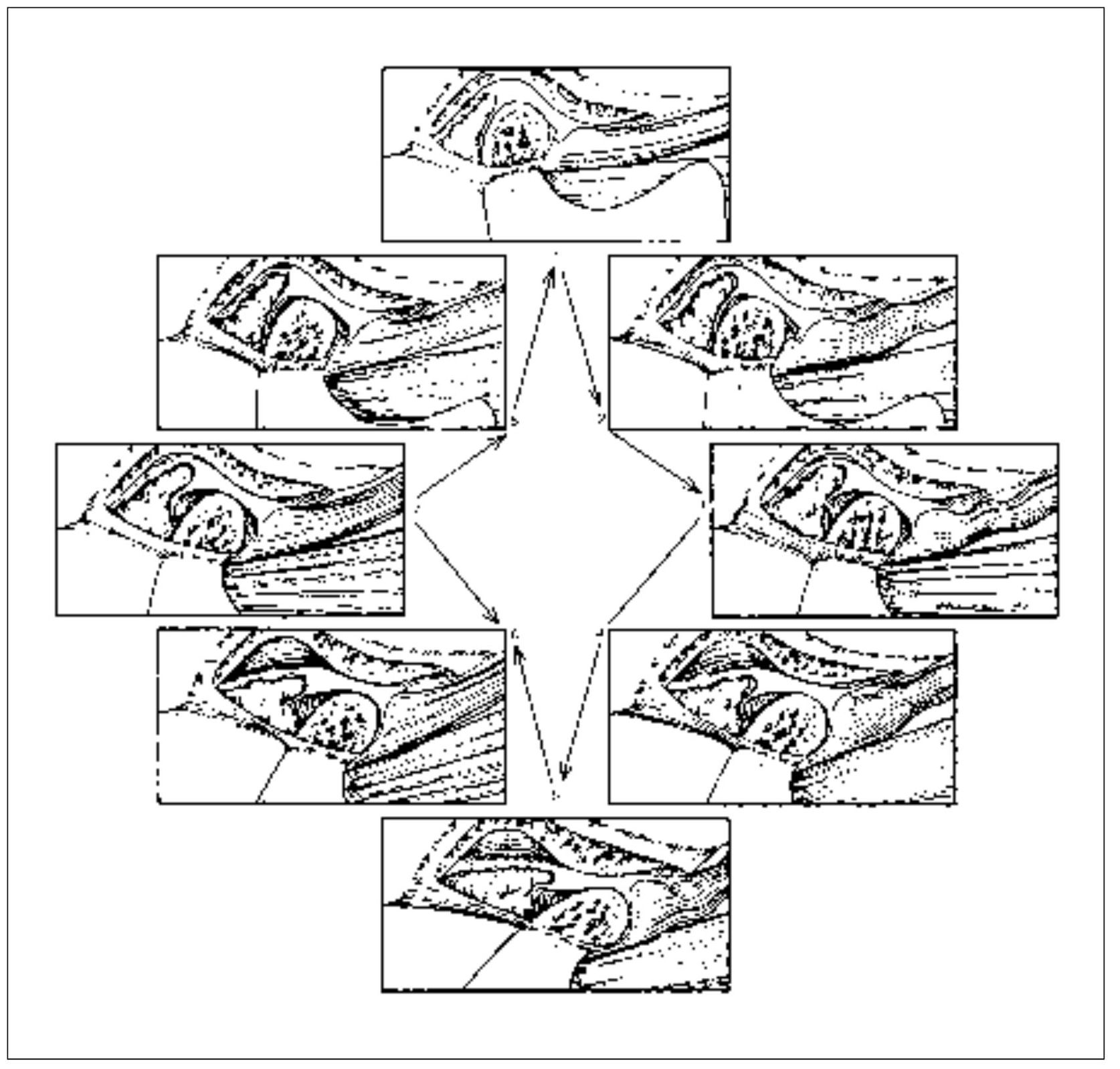
Fig 13-4 Normal functional movement of the condyle and disc during the full range of opening and closing. Note that the disc is rotated posteriorly on the condyle as the condyle is translated out of the fossa. The closing movement is the exact opposite of opening. (From Okeson JP. Management of Temporo-mandibular Disorders and Occlusion, ed 5. St Louis: Mosby-Year Book, 2003:26. Used with permission.)
Normally, the thinnest portion of the disc is centered on the condyle when the interarticular space is minimal, as during maximum intercuspation. Biting on one side against a bolus of food depresses the condyle on the ipsilateral side and widens the articular space. When this occurs, the disc is rotated anteriorly by the superior lateral pterygoid muscle, which contracts in conjunction with elevator muscle action. Thus, the thicker posterior part of the disc firmly fills the articular disc space, and adequate stability of the joint is maintained. Then, as the teeth bite through the bolus and the space narrows accordingly, the disc contour causes it to rotate posteriorly, thereby bringing the thinner portion of the disc back into position. It becomes fully centered when maximum intercuspation is accomplished. As the resting position is assumed, the space increases, with compensating rotation of the disc anteriorly as the result of muscle tonus in the resting superior lateral pterygoid muscle. This permits synovial fluid to bathe the surfaces from which it was expelled by pressure during the biting effort.
Subtle but essential disc rotary movement is constantly going on. This is in addition to that necessary for keeping the upper surface of the disc in proper contact with the eminence during translatory movement, as well as for gross separation of the jaws for opening. The more steeply inclined the articular eminence, the greater the disc movement required for condylar translation.4
Types of TMJ Pains
Arthralgic pain that emanates from a nonarticular structures of the TMJ must arise from structures that are innervated, namely, the collateral discal ligaments, the retrodiscal tissue, and the joint capsule itself, which includes the strong temporo-mandibular (lateral) ligament that reinforces its lateral wall.4 Therefore, depending on the structure from which the pain emanates, nonarticular temporomandibular arthralgia may be identified as ligamentous pain, retrodiscal pain, or capsular pain—or some combination of the three. Arthritis comprises a fourth source of arthralgia that may be identified as arthritic pain.
The ligamentous structures of the joint are innervated for proprioceptive function. They therefore are particularly responsive to such biomechanical factors as pressure, traction, stress, strain, torque, and movement. If such mechanical influence becomes noxious, pain results.5 It should be noted that both proprioceptive and nociceptive responses are dependent upon the presence of normal neural structures.6 As ligamentous deterioration takes place, the proprioceptive response and the pain diminish. It is a paradox that decreasing pain emanating from such structures may be indicative of a worsening condition of the ligaments from which it arises. It is important that this be kept in mind when evaluating the seriousness of joint pains. It should also be noted that proprioceptive responses are answered by skeletal muscle activity. Muscle co-contraction is a normal protective reaction of muscles in response to altered proprioceptive input. Therefore, muscle pain of the protective co-contraction type may accompany noxious biomechanical forces that affect the joint. Again, such response depends on normal innervation of the ligamentous structures of the joint. Acute muscle effects are indicative of normally functioning proprioceptors and therefore identify a lesser degree of deterioration in the ligaments. As deterioration takes place due to continued functional abuse and trauma, such muscle effects are less likely to occur.
It should be recognized that masticatory pain emanates from masticatory muscles, from pain-sensitive structures of the TMJs, or from both. Effective therapy depends on accurate identification of the pain source. It is therefore of considerable importance that the clinician should not only distinguish myalgia from arthralgia, but the type of myalgia or arthralgia must be correctly identified (see chapter 12 for a description of the diagnostic categories of muscle pain disorders). Arthralgia emanating from the TMJs may be classified as ligamentous pain, retrodiscal pain, capsular pain, and/or arthritic pain.
Ligamentous Pain
Pain originating from the ligamentous attachments of the condyle-disc complex may present as a range of conditions, some of which can be viewed as a continuum of progressive events. They occur secondary to changes in the relationship between the articular disc and the condyle. These conditions are often referred to as disc-interference disorders or internal derangement disorders.
If the morphology of the disc is altered and the discal ligaments become elongated, the disc is then permitted to slide (translate) across the articular surface of the condyle. This type of movement is not present in the healthy TMJ. Its degree is determined by changes that have occurred in the morphology of the disc and the degree of elongation of the discal ligaments.
Assume for the purposes of this discussion that the discal ligaments become elongated. (Ligaments can be only elongated—they cannot be stretched. Stretch implies extension that is followed by a return to the original length. Ligaments do not have elasticity and therefore, once elongated, generally remain at that length.) In the normal closed-joint position and during function, interarticular pressure still allows the disc to position itself on the condyle, and no unusual symptoms are noted. However, alteration in the morphology of the disc accompanied by elongation of the discal ligaments can change this normal functioning relationship. In the resting closed-joint position, the interarticular pressure is very low. If the discal ligaments become elongated, the disc is free to move on the articular surface of the condyle. Since in the closed-joint position the superior retrodiscal lamina does not provide much influence on disc position, tonicity of the superior lateral pterygoid will encourage the disc to assume a more forward position on the condyle. The forward movement of the disc will be limited by the length of the discal ligaments, the inferior retrodiscal lamina, and the thickness of the posterior border of the disc. As this area is thinned, the disc may be displaced more in the anteromedial direction. Since the superior retrodiscal lamina provides little residence in the closed-joint position, the medial and anterior position of the disc is maintained. As the posterior border of the disc becomes thinned, it can be displaced further into the discal space, so that the condyle becomes positioned on the posterior border of the disc. This condition is known as functional disc displacement (Figs 13-5a to 13-5c). Most persons report functional displacements of the disc initially as a momentary altered sensation during movement, but not usually as pain. Pain may occasionally be experienced when the person bites (a power stroke) and activates the superior lateral pterygoid. As this muscle pulls, the disc is displaced further, and tightness in the already elongated discal ligament can produce joint pain.
With the disc in this more forward and medial position, function of the joint can be somewhat compromised. As the mouth opens and the condyle moves forward, a short distance of translatory movement can occur between the condyle and the disc until the condyle once again assumes its normal position on the thinnest area of the disc (intermediate zone). Once it has translated over the posterior surface of the disc to the intermediate zone, interarticular pressure maintains this relationship, and the disc is again carried forward with the condyle through the remaining portion of the translatory movement. After the full forward movement is completed, the condyle begins to return and the stretched fibers of the superior retrodiscal lamina actively assist in returning the disc with the condyle to the closed-joint position. Again, the interarticular pressure maintains the articular surface of the condyle on the intermediate zone of the disc by not allowing the thicker anterior border to pass between the condyle and the articular eminence.
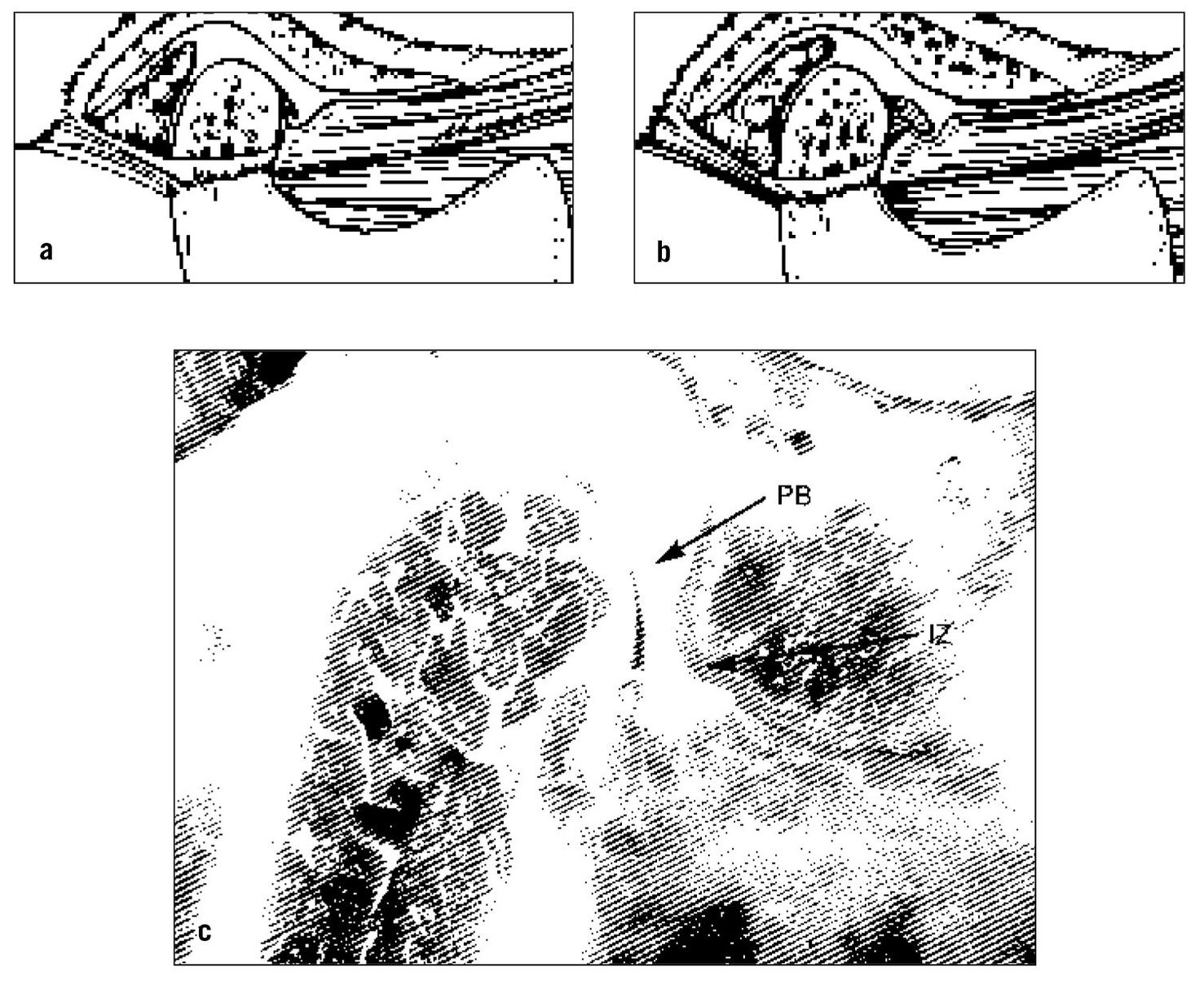
Fig 13-5 (a) Normal position of the disc on the condyle in the closed-joint position. (b) Functional displacement of the disc. Note that its posterior border has been thinned and the discal and inferior retrodiscal ligaments are elongated, allowing activity of the superior lateral pterygoid to displace the disc anteriorly (and medially). (c) Note that in this specimen the condyle is articulating on the posterior band of the disc (PB) and not on the intermediate zone (IZ). This depicts an anterior displacement of the disc. (From Okeson JP. Management of Temporomandibular Disorders and Occlusion, ed 5. St Louis: Mosby-Year Book, 2003:207. Used with permission.)
Once in the closed-joint position, again the disc is free to move according to the demands of its functional attachments. The presence of muscle tonicity will again encourage the disc to assume its most anteromedial position allowed by the discal attachments and its own morphology. One can imagine that if muscle hyperactivity was present (as with bruxism), the superior lateral pterygoid would have even a greater influence on the disc position.
The important feature of this functional relationship is that the condyle translates across the disc to some degree when movement begins. This type of movement does not occur in the normal joint. During such movement the increased interarticular pressure may prevent the articular surfaces from sliding across each other smoothly. The disc can stick or be bunched slightly, causing an abrupt movement of the condyle over it into the normal condyle-disc relationship. Often, a clicking sound accompanies this movement. Once the joint has clicked, the normal relationship of the disc and condyle is re-established, and this relationship is maintained during the rest of the opening movement. During closing of the mouth, the normal relationship of the disc and condyle is maintained because of interarticular pressure. However, once the mouth is closed and the interarticular pressure is lower, the disc can once again be displaced forward by tonicity of the superior lateral pterygoid muscle. In many instances, if the displacement is slight and the interarticular pressure is low, no click is noted during this redisplacement. This single click observed during opening movement represents the very early stages of disc-derangement disorder or what is also called internal derangement.
If this condition persists, a second stage of derangement can arise. As the disc is more chronically positioned forward and medially by muscle action of the superior lateral pterygoid and normal opening and closing, the discal ligaments can be further elongated. Continued forward positioning of the disc also causes elongation of the inferior retrodiscal lamina. Accompanying this breakdown is a continued thinning of the posterior border of the disc, which permits the disc to be positioned more anteriorly, resulting in a more posterior positioning of the condyle on the posterior border.7 The morphologic changes of the disc at the area where the condyle rests can create a second click during the later stages of condylar return, just prior to reaching the closed-joint position. This closing click is called the reciprocal click8 (Fig 13-6).
The opening click can occur at anywhere during that movement, depending on disc-condyle morphology, muscle pull, and the pull of the superior retrodiscal lamina. The closing click almost always occurs very near the closed or intercuspal position.
It should be remembered that the longer the disc is anteriorly displaced, the more the superior retrodiscal lamina are being elongated. If this condition is maintained for a prolonged period, the elasticity of the superior retrodiscal lamina can break down and be lost. It is important to remember that the superior retrodiscal lamina is the only structure that can apply retractive force on the disc, even though the retractive force is very minimal in the closed-mouth position. Once this force is lost, there is no mechanism to retract the disc posteriorly.
Some authors9 debate the role of the superior lateral pterygoid muscle on the anterior medial displacement of the disc. Although this would appear to be the obvious influencing factor, certainly other features need to be considered. Tanaka10,11 has identified a ligamentous attachment of the medial portion of the condyle-disc complex to the medial wall of the fossa. If this ligament were tightly bound, forward movement of the condyle could create a tethering of the disc to the medial. Tanaka12 has also identified that the retrodiscal tissues are tightly attached in the medial aspect of the posterior fossa, but not in the lateral aspect. This might suggest that the lateral aspect of the disc can be more easily displaced then the medial, allowing the direction of the disc displacement to be more anteromedial. There are likely other factors that have not yet been described. Further investigation in this area is needed.
With this in mind, we can now begin a discussion of the next stage of disc derangement. Remember that the longer the disc is displaced anteriorly and medially, the greater will be the thinning of its posterior border and the more the lateral discal ligament and inferior retrodiscal lamina will be elongated. Also, protracted anterior displacement of the disc leads to a greater loss of elasticity in the superior retrodiscal lamina. The more the shape of the disc changes to accommodate the pull of the muscle and the position of the condyle, the greater the likelihood that the disc will be forced through the discal space, collapsing the joint space behind. In other words, if the posterior border of the disc becomes more thinned, the disc can move even more anteromedially and actually pass completely through the discal space. When this occurs, interarticular pressure will collapse the discal space, trapping the disc in the forward position. Then the next full translation of the condyle is inhibited by the anterior and medial position of the disc. The person feels the joint being locked in a limited closed position. Since the articular surfaces have actually been separated, this condition is referred to as a functional dislocation of the disc (Figs 13-7a to 13-7c).
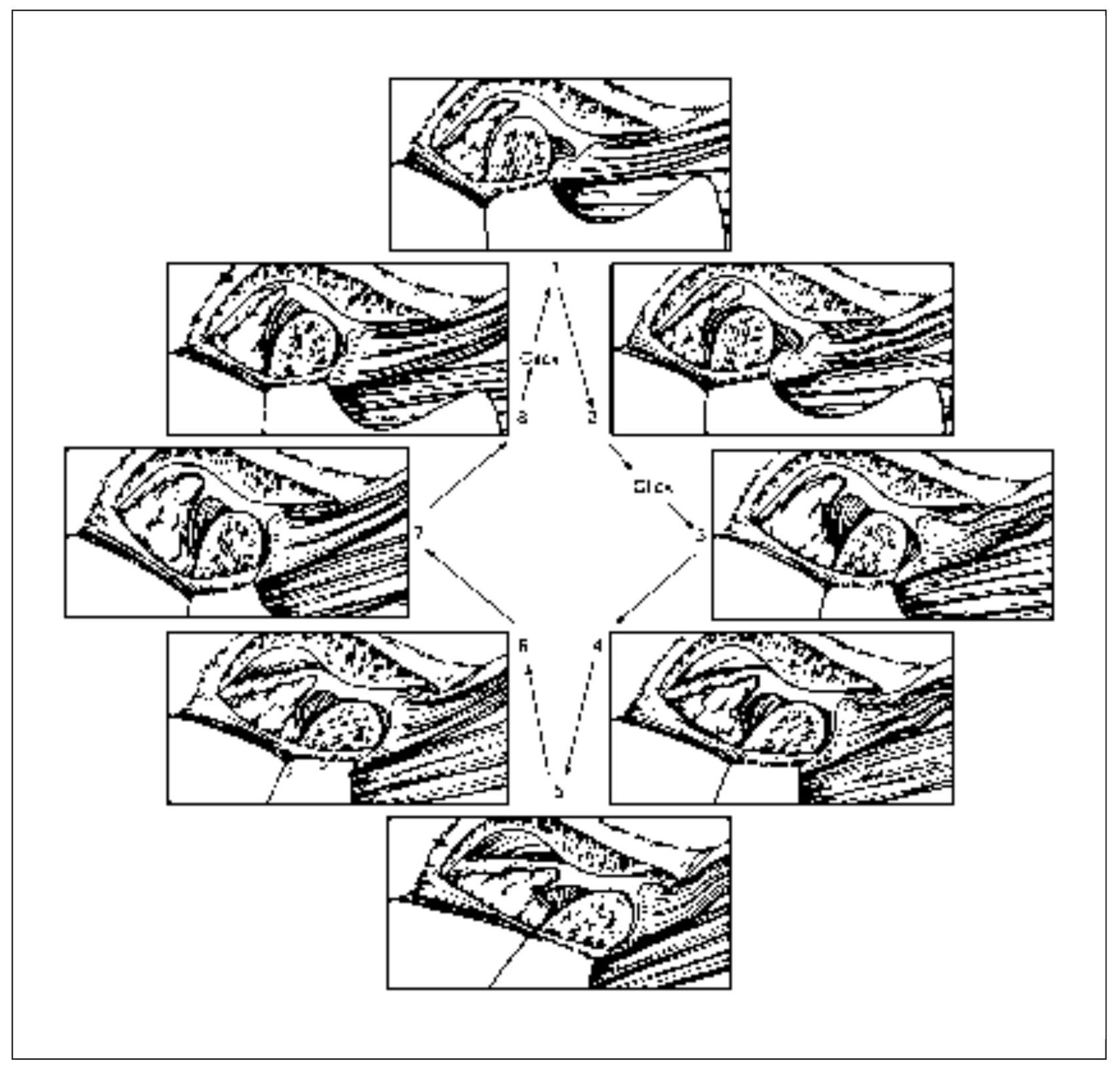
Fig 13-6 Reciprocal click. Between positions 2 and 3, a click is felt as the condyle moves across the posterior border of the disc. Normal condyle-disc function occurs during the remaining opening and closing movement until the closed-joint position is approached. Then a second click is heard as the condyle once again moves from the intermediate zone to the posterior border of the disc (between positions 8 and 1). (From Okeson JP. Management of Temporomandibular Disorders and Occlusion, ed 5. St Louis: Mosby-Year Book, 2003:210. Used with permission.)
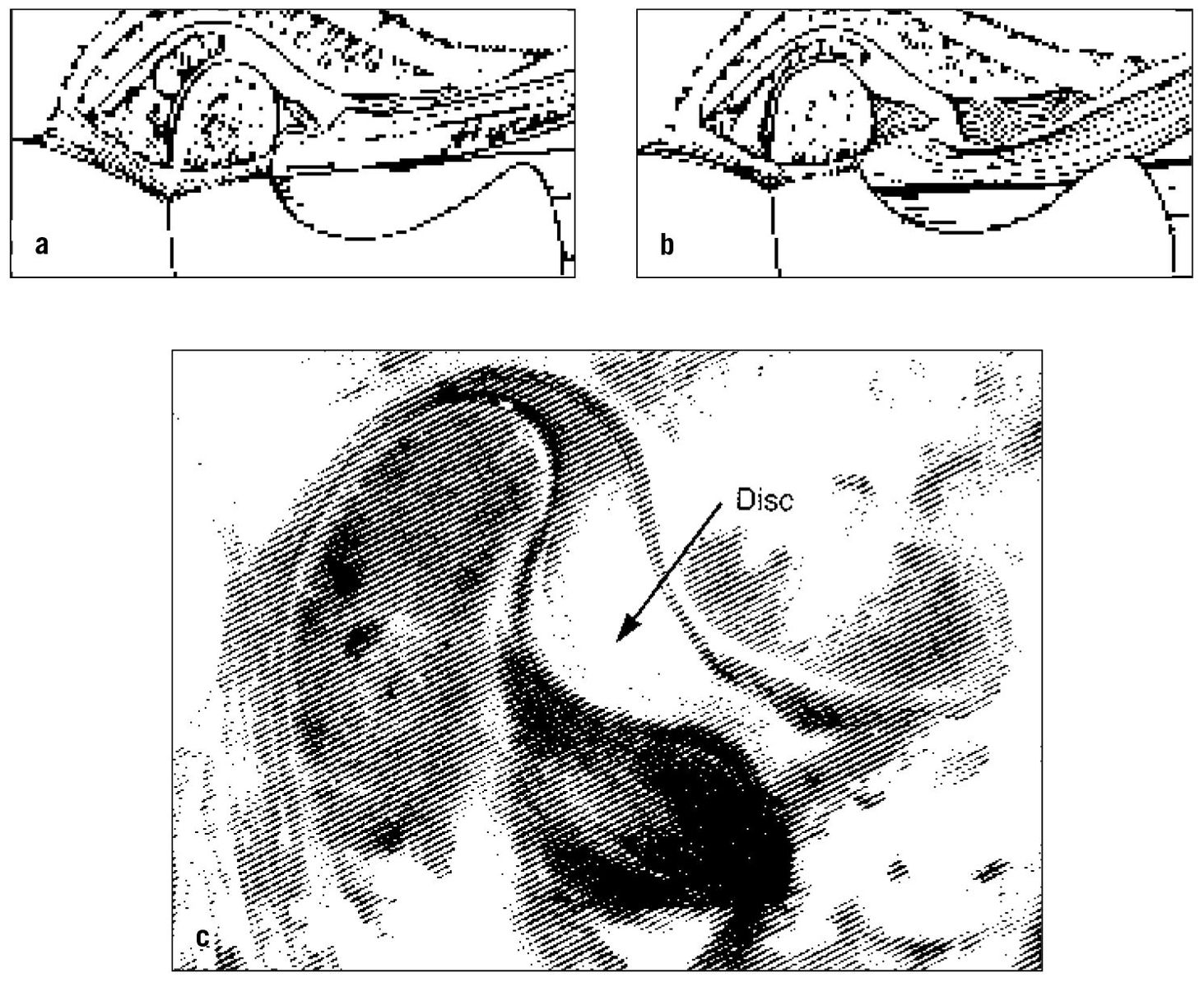
Fig 13-7 (a) Functionally displaced disc; (b) functionally dislocated disc. Note that in the functionally dislocated disc the joint space has narrowed and the disc is trapped anteriorly (and medially). (c) Note that in this specimen the disc is functionally dislocated anterior to the condyle. (From Okeson JP. Management of Temporomandibular Disorders and Occlusion, ed 5. St Louis: Mosby-Year Book, 2003:212. Used with permission.)
As already described, a functionally displaced disc can create joint sounds as the condyle moves across the disc during normal translation of the mandible. If the disc becomes functionally dislocated, the joint sounds are eliminated, since the condyle no longer moves onto the disc. This can be helpful information in distinguishing a functional displacement from a functional dislocation.
Some persons with a functional dislocation of the disc are able to move the mandible in various lateral directions to accommodate the movement of the condyle over the posterior border of the disc, and the locked condition is resolved. If the lock occurs only occasionally and the person can resolve it with no assistance, it is referred to as a functional dislocation with reduction (Fig 13-8). The patient will often report that the jaw “catches” when opening wide. This condition may or may not be painful depending on the severity and duration of the lock and the integrity of the structures in the joint. If it is acute, with a short history and duration, joint pain may only be associated with elongation of the joint ligaments (such as trying to force the jaw open). As episodes of catching or locking become more frequent and chronic, ligaments break down and innervation is lost. Pain becomes associated less with ligaments and is related more to forces placed on the retrodiscal tissues.
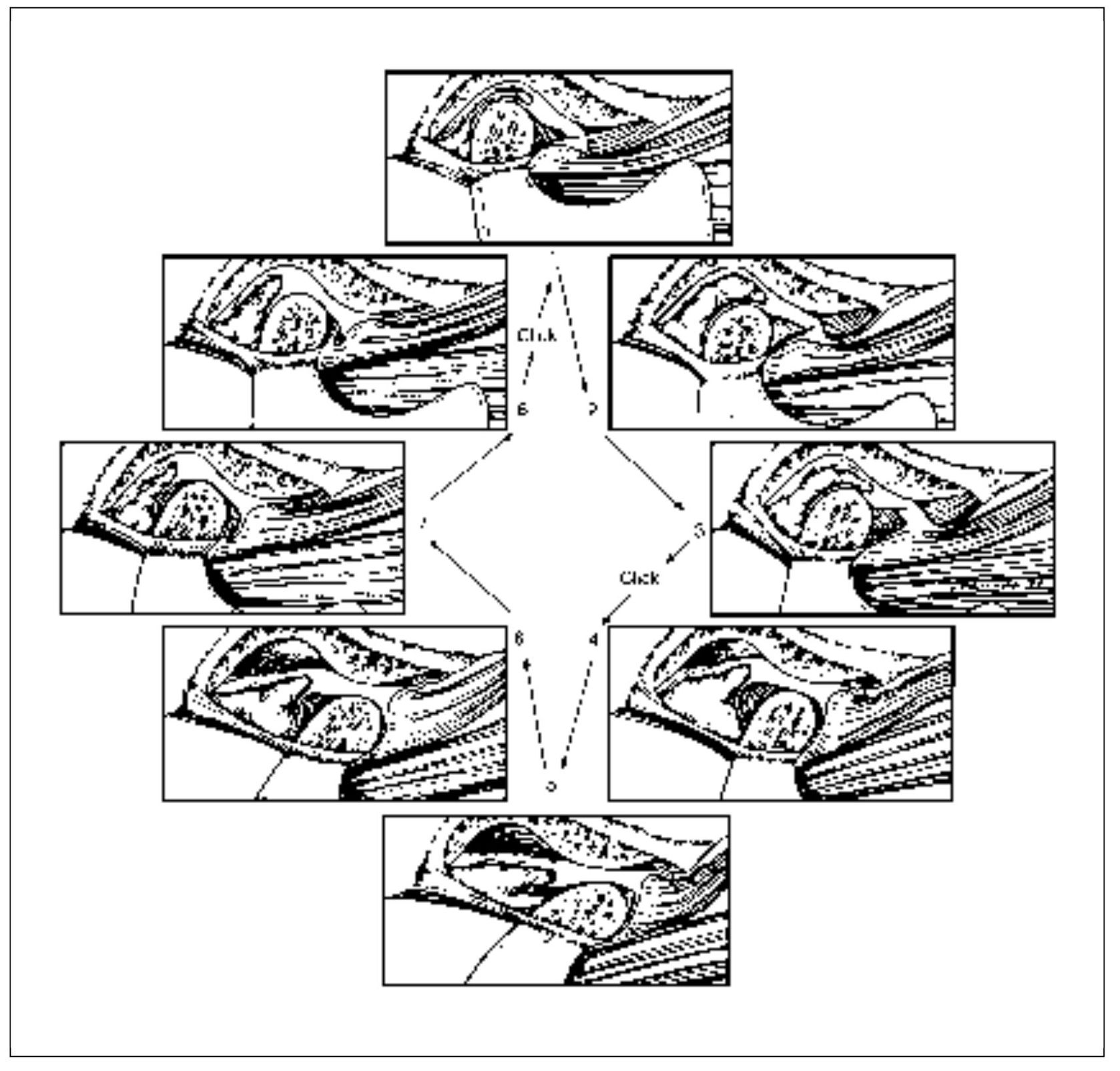
Fig 13-8 Functional dislocation of the disc with reduction. Note that during opening the condyle passes over the posterior border of the disc onto the intermediate area of the disc, thus reducing the dislocated disc. This may be felt as a “catching” sensation and is often associated with reciprocal clicking. (From Okeson JP. Management of Temporomandibular Disorders and Occlusion, ed 5. St Louis: Mosby-Year Book, 2003:213. Used with permission.)
The next stage of disc derangement is known as functional disc dislocation without reduction. This condition occurs when the person is unable to return the dislocated disc to its normal position on the condyle. The mouth cannot be open maximally because the position of the disc does not allow full translation of the condyle (Fig 13-9). Typically, the initial opening will be only 25 to 30 mm interincisally, which represents mostly the rotational movement of the joint. The person usually is aware of which joint is involved and can remember the occasion that led to the locked feeling. Since usually only one joint becomes locked, a distinct pattern of mandibular movement is observed clinically. The joint with the functionally dislocated disc without reduction does not allow complete translation of its condyle, whereas the other joint functions normally. Therefore, when the patient attempts to open wide, the midline of the mandible is deflected to the affected side. Also, the patient is able to perform a normal lateral movement to the affected side (the condyle on the affected side only rotates). However, when movement is attempted to the unaffected side, the full range of eccentric movement is not achieved (the condyle on the affected side cannot translate past the anterior functionally dislocated disc). The dislocation without reduction is also known as a closed lock. Patients may report pain when the mandible is moved to the point of limitation, but pain is not always associated with this condition.13
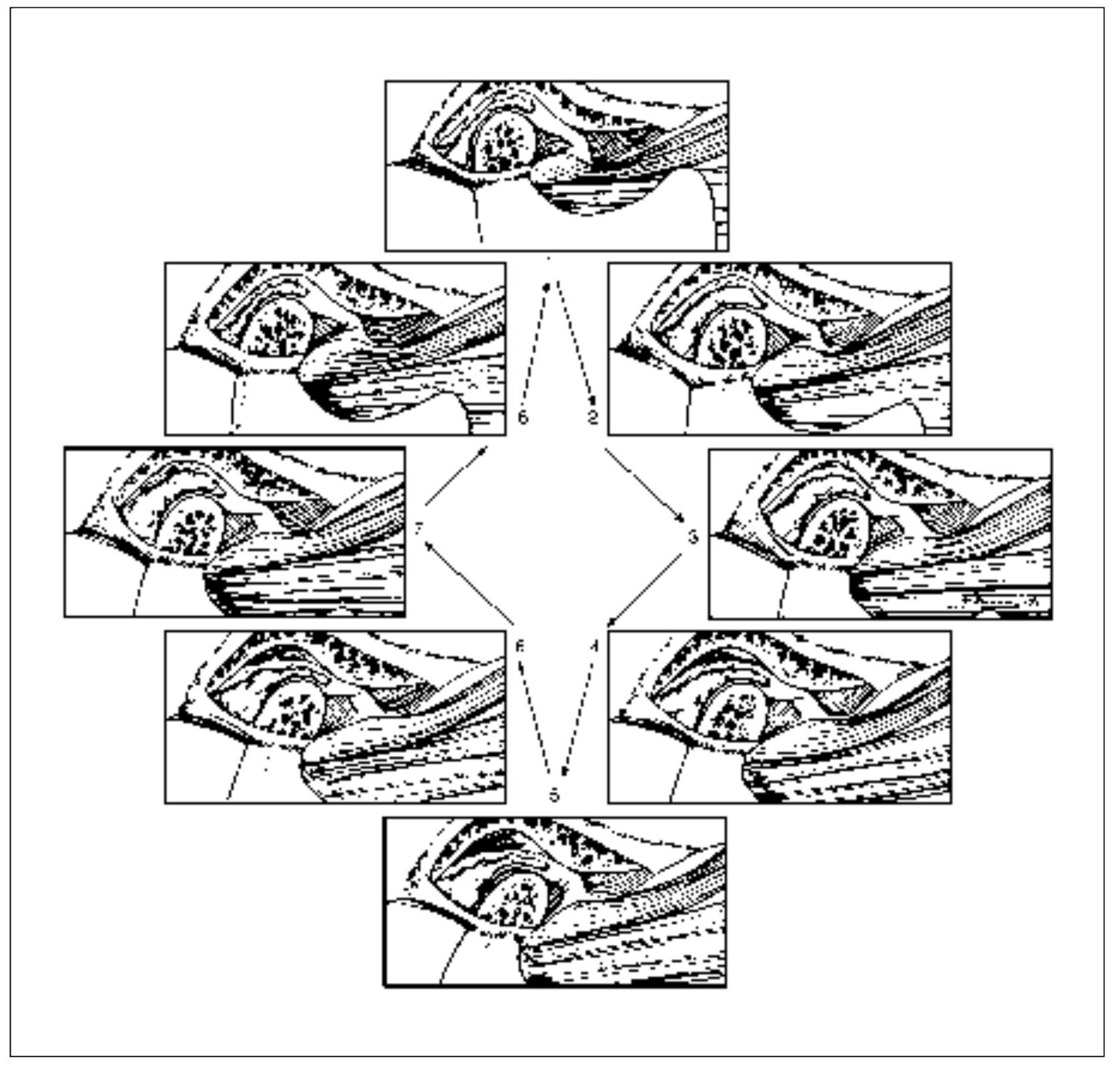
Fig 13-9 Closed lock. Note that the condyle never assumes a normal relationship on the disc but instead causes the disc to move forward ahead of it. This condition limits the distance it can translate forward. (From Okeson JP. Management of Temporomandibular Disorders and Occlusion, ed 5. St Louis: Mosby-Year Book, 2003:214. Used with permission.)
If the closed lock continues, the condyle is chronically positioned on the retrodiscal tissues. These tissues are not anatomically structured to accept force. Therefore, as force is applied, there is a great likelihood that the tissues will break down.14 With this breakdown comes tissue inflammation. This disorder will be discussed in the next category of TMJ pains.
Any condition or event that leads to elongation of the discal ligaments or thinning of the disc can cause these derangements of the condyle-disc complex disorders. Certainly one of the most common factors is trauma. Two general types of trauma need to be considered: macrotrauma and microtrauma.
Macrotrauma
Macrotrauma is considered any sudden force to the joint that can result in structural alterations. The most common structural alterations affecting the TMJ are elongation of the discal ligaments. Macrotrauma can be sub-divided into two types: direct trauma or indirect trauma.
Direct trauma
There is little question that significant direct trauma to the mandible, such as a blow to the chin, can instantly create an intracapsular disorder. If this trauma occurs when the teeth are separated (open-mouth trauma), the condyle can be suddenly displaced from the fossa. This sudden movement of the condyle is resisted by the ligaments. If the force is great, the ligaments can become elongated, which may compromise normal condyle-disc mechanics. The resulting increased looseness can lead to discal displacement and to the symptoms of clicking and catching. Unexpected macrotrauma to the jaw (as might be sustained during a fall or in a motor vehicle accident) may lead to discal displacement and/or dislocation.15,16,17,18,19,20,21,22,23,24,25
Macrotrauma can also occur when the teeth are together (closed-mouth trauma). If trauma occurs to the mandible when the teeth are together, the intercuspation of the teeth maintains the jaw position, resisting joint displacement. Closed-mouth trauma is therefore less injurious to the condyle-disc complex. This reduction of potential injury becomes obvious when one examines the incidence of injury associated with athletic activity. Athletes who wear soft protective mouth appliances have significantly fewer jaw-related injuries than those that do not.26,27 It would be wise, therefore, if facial trauma were expected, to have a soft appliance in place or at least hold the teeth tightly in the intercuspal position. Unfortunately, most direct macrotrauma is unexpected (ie, motor vehicle accident) and therefore the teeth are separated, commonly resulting in injury to the joint structures.
Closed-mouth trauma is not likely to be without some consequence. Although ligaments may not be elongated, articular surfaces can certainly receive sudden traumatic loading.28 This type of impact loading may disrupt the articular surface of the condyle, fossa, or disc, which may lead to alterations in the smooth sliding surfaces of the joint, causing roughness and even sticking during movement. This type of trauma therefore may result in adhesions, which will be addressed later in this chapter.
Direct trauma may also be iatrogenic. Any time the jaw is overextended, elongation of the ligaments can occur. Patients are more at risk for this type of injury if they have been sedated, reducing normal joint stabilization by the muscles. A few common examples of iatrogenic trauma are intubation procedures,29,30 third molar extraction procedures, and a long dental appointment. In fact, any extended wide opening of the mouth (eg, a yawn) has the potential of elongating the discal ligaments.15 The medical and dental professions need to be acutely aware of these conditions so as not to create a disc-derangement problem that might last the patient’s lifetime.
Indirect trauma
Indirect trauma refers to injury that may occur to the TMJ secondary to a sudden force, but not one that occurs directly to the mandible. The most common type of indirect trauma reported is associated with a cervical extension/flexion injury (whiplash injury).17,23,31,32 Although the literature reflects an association between whiplash injury and symptoms of TMJ disorders, the data are still lacking regarding the precise nature of this relationship.33,34
Recent computer modeling suggests that certain motor vehicle injuries do not produce a TMJ flexion-extension event similar to that seen in the neck.35,36 In support, human volunteers in motor vehicular crash tests fail to show jaw movement during a rear-end impact.37 Therefore, there is little compelling evidence at this time to support the concept that indirect trauma commonly results in quick movement of the condyle within the fossa, creating a soft tissue injury similar to that seen in the cervical spine.38,39 This is not to say that this type of injury could never occur—only that it is likely very rare.
If this statement is true, why then are TMJ symptoms so commonly associated with cervical spine injuries?17,23,32 The answer to this question lies in the understanding of heterotopic symptoms (chapter 4). The clinician always needs to be mindful that constant deep pain input originating in the cervical spine commonly creates heterotopic symptoms in the face.40 These heterotopic symptoms may be referred pain (sensory) and/or co-contraction of masticatory muscles (motor). Kronn32 reported that patients who experienced recent whiplash injuries have a greater incidence of TMJ pain, limited mouth opening, and masticatory muscle pain on palpation than a matched group of controls. All of these symptoms can be explained as heterotopic symptoms associated with deep pain input from the cervical spine. The clinical significance of understanding this concept is enormous, since it dictates therapy. As will be discussed in future chapters, when these circumstances occur, therapy extended to the masticatory structures will have little effect on resolving the cervical deep pain input. Primary emphasis needs to be directed to the cervical injury (the origin of the pain).
Microtrauma
Microtrauma refers to any small force that is repeatedly applied to the joint structures over a long period of time. As discussed earlier in this chapter, the dense fibrous connective tissues that cover the articular surfaces of the joints can well tolerate loading forces. In fact, these tissues need a certain amount of loading to survive, since loading forces drive synovial fluid in and out of the articular surfaces, passing with it nutrients coming in and waste products going out. If, however, loading exceeds the functional limits of the tissue, irreversible changes or damage can result. When the functional limitation has been exceeded, the collagen fibrils become fragmented, resulting in a decrease in the stiffness of the collagen network. This allows the proteoglycan-water molecules to swell and flow out into the joint space, leading to a softening of the articular surface. This softening is called chondromalacia.41 This early stage of chondromalacia is reversible if the excessive loading is reduced. If, however, the loading continues to exceed the capacity of the articular tissues, irreversible changes can occur. Regions of fibrillation can begin to develop. resulting in focal roughening of the articular surfaces.42 This alters the frictional characteristics of the surface and may lead to sticking of the articular surfaces, causing changes in the mechanics of condyle-disc movement. Continued sticking and/or roughening leads to strains on the discal ligaments during movements and eventually disc displacements.41
Another consideration regarding loading is the hypoxia/reperfusion theory. As previously stated, loading of the articular surfaces is normal and necessary for health. However, on occasion the forces applied to the articular surfaces can exceed the capillary pressure of the supplying vessels. If this pressure is maintained, hypoxia can develop in the structures supplied by the vessels. When the interarticular pressure is returned to normal, there is a reperfusion phase. It is thought that during this reperfusion phase, free radicals are released into the synovial fluid. These free radicals can rapidly break down the hyaluronic acid that protects the phospholipids that line the joint surfaces and provide important lubrication.43,44,45,46 When the phospholipids are lost,47 the articular surfaces joint no longer slide frictionless leading to breakdown. The resulting “sticking” can also lead to disc displacement. Free radicals are also associated with hyperalgesic states and can therefore produce a painful joint.48,49
Microtrauma can result from joint loading associated with muscle hyperactivity, such as bruxism or clenching.50,51 This may be especially true if the bruxing activity is intermittent and the tissues have not had an opportunity to adapt. It is likely that if the bruxing is long-standing, the articular tissues have adapted to the loading forces and changes will not be seen. In fact, in most patients, gradual loading of the articular surfaces leads to a thicker, more tolerant articular tissue.52,53,54
Another type of microtrauma results from mandibular orthopedic instability. Orthopedic stability in the masticatory system exists when the stable intercuspal position of the teeth is in harmony with the musculoskeletally stable position of the condyles.55 When this condition does not exist, microtrauma to the joint structures can result. This trauma occurs not when the teeth are initially brought into contact, but only during loading of the masticatory system by the elevator muscles. Once the teeth are in the intercuspal position, elevator muscle activity loads the teeth and the joints. Since the intercuspal position represents the most stable position for the teeth, loading is accepted by the teeth without consequence. If the condyles are also in a stable relationship in the fossae, loading occurs with no adverse effect to the joint structures. If, however, loading occurs when a joint is not in a stable relationship with the disc and fossa, unusual movement can occur in an attempt to gain stability. This movement is often a translatory shift between disc and condyle and can lead to elongation of the discal ligaments and thinning of the disc. Remember that the amount and intensity of the loading greatly influence whether the orthopedic instability will lead to a disc-derangement disorder. Bruxing patients with orthopedic instability, therefore, are more likely to create problems than non-bruxers with the same occlusion.
An important question that arises in dentistry is: “What occlusal conditions are commonly associated with disc derangements?” It has been suggested that when an occlusal condition causes a condyle to be positioned posterior to the musculoskeletally stable position, the posterior border of the disc can be thinned.56 A common occlusal condition that has been suggested to provide this environment is the skeletal Class II deep bite, which may be further aggravated when a division 2 anterior relationship also exists.57,58,59,60 One needs to be aware, however, that not all patients with Class II malocclusions present with disc-derangement disorders. Some studies show no relationship between Class II malocclusion and these disorders.61,62,63,64,65,66,67,68,69,70,71 Other studies show no association between the horizontal and vertical relationship of the anterior teeth and disc-derangement disorders.72,73,74 The important feature of an occlusal condition that leads to disc-derangement disorders is the lack of joint stability when the teeth are tightly occluded. It is likely that some Class II malocclusions provide joint stability, while others do not. Another factor that must be considered is the amount and duration of joint loading. Perhaps joint loading is more damaging with certain Class II malocclusions. It becomes obvious that no simple relationship exists. It is vitally important, however, that when orthopedic instability exists it be identified as an etiologic factor; successful management may depend on prompt alteration of the damaging relationship (Case 8).
Case 8 Temporomandibular arthralgia originating in the retrodiscal tissues
Chief Complaint Right TMJ pain.
History
A 45-year-old woman presented with mild to severe, intermittent, steady, dull, aching pain diffusely located in the right preauricular area. The pain was induced by clenching the teeth and lasted from a few minutes to an hour or longer. The pain was accompanied by sensations of interference and disc noise especially associated with occluding the teeth firmly.
The complaint began about 6 months ago. One day while chewing, she bit down firmly and sensed a locking of the right joint. As she opened, it popped very loudly and she felt severe, sharp pain in the TMJ area. The noise and pain have occurred with firmly occluding the teeth ever since. She reports that for several years prior to this, she had noisy TMJs with chewing. She presently has no complaint of restriction of mandibular movements or any recent alteration in her “bite.” She is taking no medications of any kind.
Examination
Intraoral: Clinical examination fails to identify any dental or oral cause for the pain except for the orthopedic instability provided by the occlusal condition, as indicated by sensing premature contact of the right premolars, a feeling of increased pressure on those teeth in the fully occluded position, and some movement from primary contact to the full occlusal position. She feels right preauricular pain when she clenches the teeth, and this is accompanied by a “binding sensation.” As she releases the teeth, moderate right disc noise is heard. All this is readily prevented by biting on a tongue blade. Otherwise, masticatory functioning is clinically normal.
TMJs: Both joints present clinical evidence of changes in the articular disc positions. When the condyles are positioned by bilateral manual manipulation into the musculoskeletally stable position, the teeth do not occlude soundly. When the patient is asked to fully close the teeth together, a 3-mm shift forward and to the left is noted.
Muscles: No palpable tenderness in the masticatory muscles. All functioning appears to be well within normal limits.
Cervical: Within normal limits.
Cranial nerves: Within normal limits.
Impression
The patient presents with an orthopedically unstable relationship between the stable occlusal position and the orthopedically stable position for the joints. Over the years, this instability, coupled with chewing and other loading factors, has resulted in alteration in normal condyle/disc function, leading to the joint sounds. A few months ago, she accidentally impinged the right disc with sufficient force to injure its attachments to the condyle, thus causing the symptoms of acute retrodiscitis.
Diagnosis Acute retrodiscitis of the right TMJ, as a result of intrinsic injury.
The following are clinical symptoms by which ligamentous pain can be recognized:
- The pain occurs intermittently in conjunction with clinically evident disc interference of some type.
- Pain that occurs in conjunction with condylar translatory movements relates specifically to one of the following etiologic groups of disc-interference disorders 4:
- Excessive passive interarticular pressure
- Structural incompatibility between the sliding parts
- Degeneration of the articular surfaces
- Impaired disc-condyle complex
- Protective muscle co-contraction may be displayed.
- Dysfunction in the form of interference during mandibular movements is characteristic. If such interference is sufficient to arrest condylar movement, dysfunction in the form of restricted range of motion is displayed.
- Ordinarily, central excitatory effects are not seen. (If the ligaments become inflamed, the clinical characteristics of capsular pain will be displayed. Then, secondary effects may become evident.)
Retrodiscal Pain
The retrodiscal tissues are located posterior to the articular disc and extend back to the posterior wall of the joint capsule. As previously mentioned, these tissues are composed of highly vascularized, loose connective tissue. The inferior retrodiscal lamina is composed of collagenous tissue and serves as a ligament that restricts anterior rotation of the disc on the condyle and delineates the inferior synovial sac between the articular disc and the mandibular condyle posteriorly. The superior retrodiscal lamina is composed of elastic tissue and serves not as a ligament but as a retractive force on the articular disc when the condyle is translated forward. At the closed-mouth occluded position, however, both laminae are relaxed and exert no traction on the disc. The superior retrodiscal lamina delineates the superior synovial sac between the articular disc and the tympanic plate posteriorly. The retrodiscal tissue is sometimes referred to as the posterior attachment of the disc.
Both retrodiscal laminae are surfaced with synovial membrane. The vascularity of the retrodiscal tissue is a major source of synovial fluid to both compartments of the joint. This tissue is structured so that full and extensive translatory movements of the condyle do not interfere with the continuous flow of nutrients and metabolic exchange supplying the nonvascularized articular surfaces and articular disc. The retrodiscal tissue is innervated, as is other loose connective tissue, with somatic and visceral afferents, including nociceptors, and with visceral efferents to the blood vessels. 6 It has little or no proprioceptive capability; its chief function is nutritional.
The vital retrodiscal tissue is not subject to injury under normal conditions of mandibular function. If condylar encroachment does occur, inflammation may take place. This is marked by extensive swelling, extravasation of inflammatory fluid into the synovial spaces, and pain, especially when the condyle presses against the swollen tissue during maximum intercuspation. Trauma to the mandible can therefore induce an acute retrodiscitis. Such a condition causes an acute malocclusion in the resting occluded position due to swelling of the retrodiscal tissue and excessive intracapsular fluid. The pain that occurs when the teeth are firmly occluded may be reduced considerably by biting against a separator that prevents intercuspation of the teeth. There may be some accentuation of pain when forceful ipsilateral excursions are made (Case 9).
It should be noted that retrodiscitis displays symptoms that may be misdiagnosed as inferior lateral pterygoid muscle pain or as disc attachment (ligamentous) pain due to orthopedic instability that occurs when the teeth are clenched in maximum intercuspation. It is important that these conditions be differentiated because the treatment is not the same. Inferior lateral pterygoid muscle pain is identified by increased pain with resisted protrusive effort. Disc attachment pain due to orthopedic instability displays no acute malocclusion in the resting occluded position. It should be noted, however, that radiographically these three conditions may appear much the same. Radiographic evidence therefore should not be accepted as conclusive unless it is confirmed by clinical symptoms.
The possibility of acute retrodiscitis should be considered in traumatic incidents that involve the mandible, both with and without osseous fracture (Case 9). The symptoms may be misdiagnosed as a mandibular fracture when none exists. Therapy should also take into consideration the possibility of hemarthrosis, which presents the chance of adhesions between the disc and temporal fossa (fibrosis ankylosis) or between the disc and condyle.
An insidious chronic form of retrodiscitis may occur as the result of functional encroachment of the condyle on the retrodiscal tissue due to orthopedic instability that displaces the condyle posteriorly when the teeth are firmly clenched in maximum intercuspation. The resultant deterioration in the discal ligaments, the disc proper, and the temporomandibular ligament permits condylar encroachment on the retrodiscal tissue. Such a condition comes on slowly, so that inflammatory changes sufficient to elicit symptoms usually do not occur. Such condylar encroachment involves the inferior retrodiscal lamina first, then the body of retrodiscal tissue. This usually leaves the vital superior retrodiscal lamina to function within normal limits. As metaplasia converts the retrodiscal loose connective tissue into a denser fibrotic tissue, the decreased vascularity may affect the metabolism of the synovial fluid. This may further complicate the already difficult problem of functional displacement of the articular disc upon which the retrodiscal condition is superimposed. If the matter of functional displacement proceeds to the point of anterior dislocation of the articular disc, biting pressure of the condyle against the remaining unprotected retrodiscal tissue may induce retrodiscal pain.
Case 9 Acute retrodiscitis secondary to trauma
Chief Complaint Left TMJ area pain.
History
A 46-year-old woman presented with mild, intermittent, steady, dull, aching pain diffusely located in the left preauricular area induced by clenching the teeth and accompanied by acute malocclusion, described as premature contact of the right anterior teeth with disclusion of the posterior teeth unless forced into full occlusion.
The complaint began a week ago following an automobile accident in which she sustained a heavy blow to the right chin. Radiographs failed to identify a mandibular fracture. Because of the acute malocclusion, the oral surgeon was suspicious of an unidentified fracture and placed arch bars and inter-arch elastics to bring the teeth into normal occlusion. In doing so, however, pain increased until it became intolerable, and he was forced to remove the maxillomandibular elastics and refer the patient for a TMJ examination. Only ibuprofen was being taken for the pain.
Examination
Intraoral: There is no dental or oral cause for the complaint other than the obvious acute malocclusion. Deep tenderness in the left joint is sensed with heavy manual palpation, and this increases considerably with forced occlusion of the teeth. There is slight discomfort with maximum opening and extended lateral and protrusive movements, and the patient senses a feeling of muscular weakness with these movements as well as with attemp/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


