Chapter 13
Preprosthetic and Oral Soft Tissue Surgery
Preprosthetic surgery is the surgery that aims to improve tissue conditions for later prosthetic treatment. Earlier in the history of dentistry this meant surgery aiming at increasing the base for stability and retention of removable dentures. However, today the scope of preprosthetic surgery has changed to include also the improvement of the conditions for implant treatment. Nowadays, implant treatment is an increasingly chosen option. For these reasons, this chapter aims to cover both preprosthetic surgery prior to removable dentures and conditions improving the tissue around implants. Moreover, some other simple soft tissue surgical procedures aiming at improving functions and esthetics are covered. However, crestal preparation by bone augmentation prior to implant treatment is covered in Chapters 15–18.
Surgical Methods for Alveolar Crest Preservation
Already during extraction the clinician should be aware of the importance to preserve the alveolar bone crest. Conventional extraction methods may sometimes be traumatic and cause alveolar bone destruction during the healing period. In order to avoid postextraction bone and soft tissue loss, tooth removal may be performed by tissue preserving techniques such as the use of periotome (Fig. 13.1). Bone removal should be avoided or limited, especially the marginal bone to enable later implant installation. Removal of diverging roots can be carried out by first separating them by burs instead of sacrificing bone. Another method of preserving the bone is to remove the roots following drilling them from inside, starting from the pulp chamber. Teeth that have become ankylosed after replantation shall not be removed but left for osseous replacement by bone to preserve the bone crest for later implant placement. Decoronation of the ankylosed root is a good alternative, which will leave the root for osseous replacement, thereby saving the alveolar process.

When multiple extractions are carried out, there may be postextraction irregularities of the alveolar sockets. The irregular surface may be trimmed with a bur, a rongeur, a fine osteotome or a bone file. Whenever possible, it is better to use a file or rongeur in minor discrepancies to prevent decrease of alveolar height. Various methods for preparation of the crest prior to implant treatment are ridge splitting, filling the extraction socket with biomaterials, membrane techniques and distraction osteogenesis, some of which will be covered in Chapters 15–18.
Surgical Management of Peri-Implant Soft Tissue
Implant-Related Indications
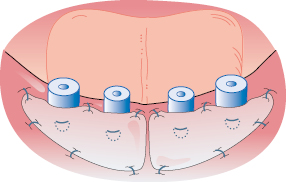
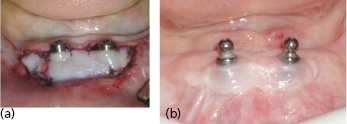
Preservation of healthy peri-implant soft tissue is an important and challenging part of dental implant treatment. The keratinized attached gingiva seems to be an important factor to avoid inflammation and peri-implantitis and for achieving the best esthetics, especially important in the anterior region. This can be achieved during surgery by planning incisions and by tight adaptation of the soft tissue to the marginal section of a dental implant, forming a natural soft tissue barrier. In an edentulous area a crestal incision is widely used to facilitate soft tissue adaptation around necks of non-submerged implants (Figs 13.2 and 13.3). The incisions should be placed at the crestal level in order to leave adequate amounts of keratinized and well-perfused mucosa at both buccal and lingual sites.
Regeneration
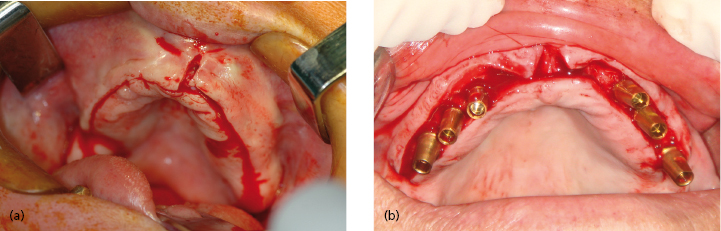
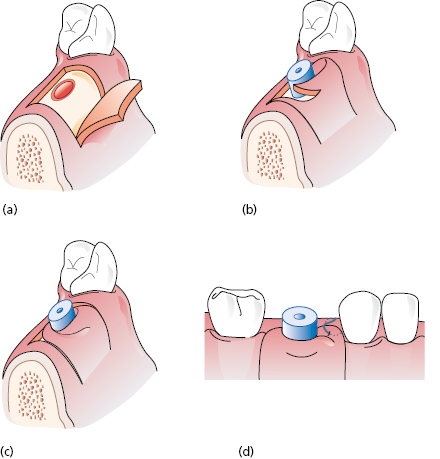
The papilla regeneration technique is a simple and innovative method to form a new papilla between implants or teeth. A small palatal or lingual crestal incision is made to uncover the implant and, immediately after a healing cap is inserted, a semilunar incision is performed in the keratinized gingiva and the tissue rotated interproximally to form a new papilla (Fig. 13.4).
Oral Soft Tissue Grafting
Sometimes it may be advantageous to graft keratinized gingiva to increase the width of the attached gingiva of the implant site. The host region should provide proper vascularization properties for graft integration. Grafts can be taken from the palatal mucosa and subepithelial connective tissue can be used to augment concavities.
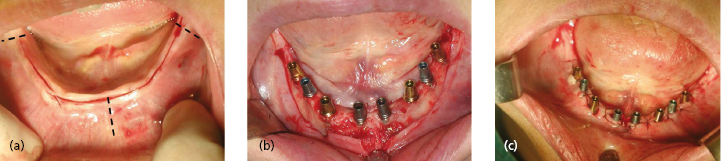
Palatal Mucosa Grafting
Mucosal palatal grafts has been used successfully for years in periodontal practice to cover denuded roots. A similar philosophy can be applied to the soft tissue around dental implants in situations with loose alveolar mucosa. Attached keratinized gingiva can be grafted from the palate. Restoration of a wide band of attached gingiva around dental implants can be seen in Figures 13.5 and 13.6.