Dental Erosion
Ann‐Katrin Johansson, Inga B. Arnadottir, Göran Koch, and Sven Poulsen
Over the past decades the dental community has shown an increasing concern about erosive tooth wear, especially in children and adolescents. This anxiety is based on clinical observations, together with reports from many countries suggesting not only a high prevalence, but also a possible increase of both occurrence and severity of dental erosion. In the young individual the literature points to the global rise in soft‐drink consumption as the most significant factor in the development of dental erosion. Other factors such as lifestyle changes, a strong perception of the importance of body image for success, and chronic diseases are other possible reasons for an increasing prevalence of dental erosion. Tooth wear has a multifactoral etiology and is a result of concurrent action of different mechanisms and factors on the teeth in the oral environment. Dental erosion is one of these components and defined as a loss of tooth substance by a chemical process that does not involve bacteria. Besides erosion, dental attrition and abrasion may occur at the same or at different occasions, which adds to the complexity of the phenomenon of wear.
Studies have shown that without presoftening by acid of the dental hard tissue the wearing effect from attrition and abrasion is reduced greatly. Dental erosion is therefore regarded as the most important factor in the development of tooth wear and attrition, and abrasion considered to be of less significance [1]. Another term used in connection with dental wear is abfraction, a combination of erosion and stress in the buccal area of the cemento–enamel region provoking micro fractures (Box 13.1).
Prevalence
Recent studies claim a high and increasing prevalence of erosions in children and adolescents. Comparison of these studies is often difficult since the diagnostic criteria, scoring systems, and choice of teeth and surfaces to be scored vary. However, there are sufficient studies to give a general idea of the prevalence and distribution of erosion both in the primary and in the young permanent dentition (Table 13.1).
Table 13.1 Prevalence of dental erosion in children (primary teeth) and adolescents (permanent teeth) in different countries. Prevalence denotes erosive damage reaching the dentin or close to dentinal exposure of large surfaces
| Country | Age (years) | No. of individuals | Prevalence (%) | Authors (year) |
| Children | ||||
| UK | 4–5 | 178 | 30 | Millward et al. (1994) |
| UK | 5 | >1000 | 24 | Downer (1995) |
| UK | 1.5–4.5 | 1658 | 8 | Moynihan & Holt (1996) |
| Saudi Arabia | 5–6 | 354 | 34 | Al‐Majed et al. (2002) |
| Ireland | 5 | 202 | 21 | Harding et al. (2003) |
| India | 5–6 | 100 | 30 | Deshpande et al. (2005) |
| Germany | 2–7 | 463 | 13 | Wiegand et al. (2006) |
| Sweden | 5–6 | 135 | 13 | Hasselkvist et al. (2010) |
| Adolescents | ||||
| UK | 14 | 1035 | 30 | Milosevic et al. (1994) |
| UK | 15 | >1000 | 2 | Downer (1995) |
| Saudi Arabia | 20 | 95 | 16 | Johansson et al. (1996) |
| Cuba | 12 | 1010 | 17 | Kunzel et al. (2000) |
| Saudi Arabia | 12–14 | 862 | 26 | Al‐Majed et al. (2002) |
| Iceland | 15 | 278 | 22 | Arnadottir et al. (2003) |
| UK | 14 | 1308 | 13 | Dugmore et al. (2003) |
| UK | 14 | 2351 | 53 | Bardsley et al. (2004) |
| Turkey | 11 | 153 | 28 | Caglar et al. (2005) |
| Denmark | 15–17 | 558 | 1.6 | Larsen et al. (2005) |
| Sudan | 12–14 | 157 | 22 | El Karim et al. (2007) |
| Iceland | 12 | 757 | 16 | Arnadottir et al. (2010) |
| Iceland | 15 | 750 | 31 | Arnadottir et al. (2010) |
| Norway | 16–18 | 795 | 15 | Søvik et al. (2014) |
| Sweden | 13–14 | 227 | 12 | Hasselkvist et al. (2010) |
| Sweden | 18–19 | 247 | 22 | Hasselkvist et al. (2010) |
| Sweden | 20 | 494 | 18 | Isaksson et al. (2014) |
The prevalence of erosion involving dentin in children aged 2–7 years has been reported to vary from 8 to 34%, while erosion limited to the enamel is definitely more frequent. Most reported studies in the young permanent dentition are carried out in adolescents aged 11–20 years and the prevalence of erosion in dentin varies from 2 to 53%. Longitudinal studies indicate an increased number of teeth being affected by erosion and also an increase in severity with increasing age.
Distribution of dental erosion
The distribution of dental erosion is not uniform within the dental arches. Studies have shown that it is not possible to predict exactly the localization of such lesions depending on their etiology [2]. It is, however, clear that erosion will affect some teeth more than others. In children and adolescents, the maxillary anterior teeth, especially the palatal surfaces, and permanent first molars are those most often affected. The distribution of dental erosion in 12‐ and 15‐year‐old boys and girls are shown in Figure 13.1(a,b). The highest frequencies of erosion, both in boys and girls, were found in the mandibular first molars. The figures indicate an increased prevalence of erosion at age 15 compared with 12 years of age.
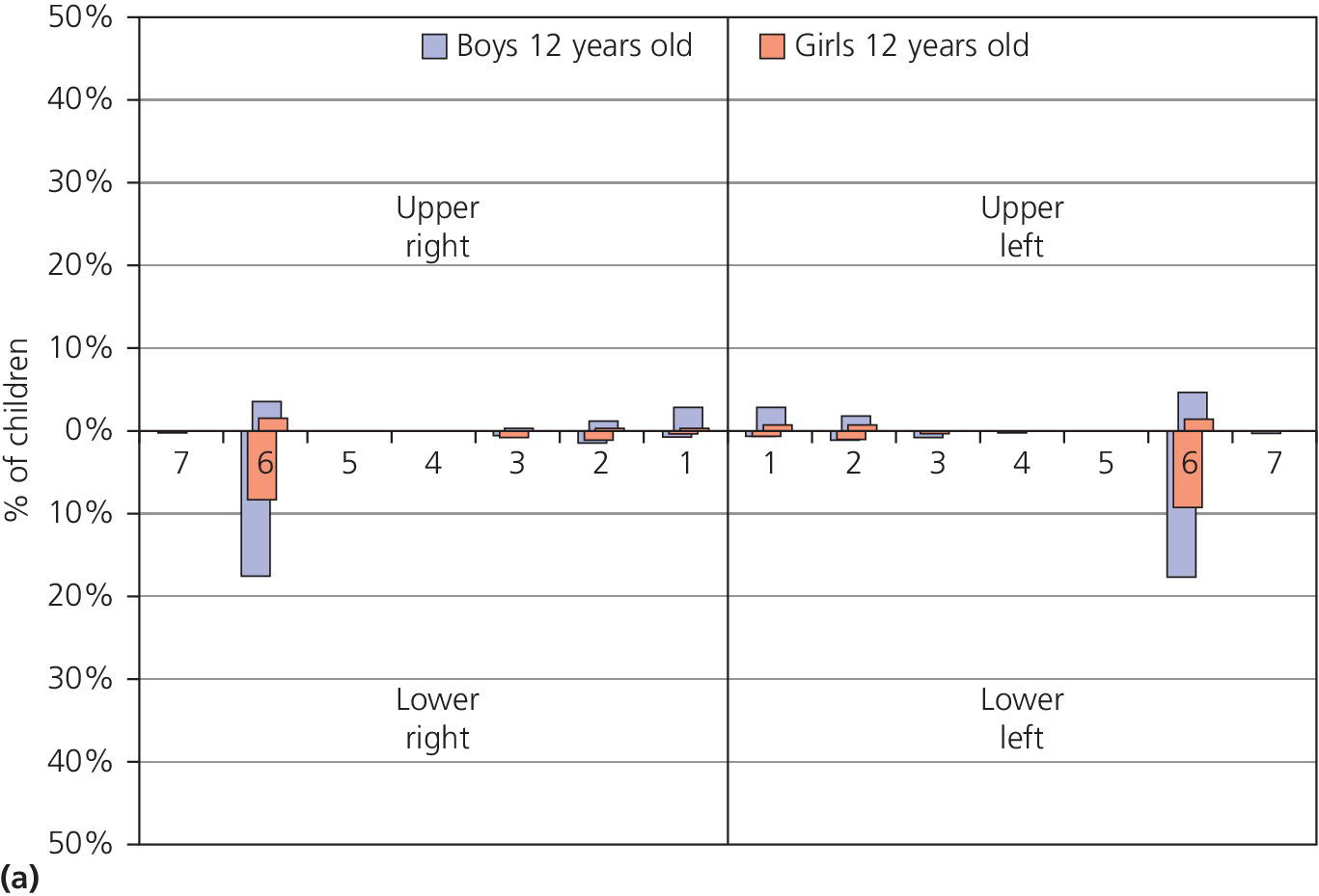
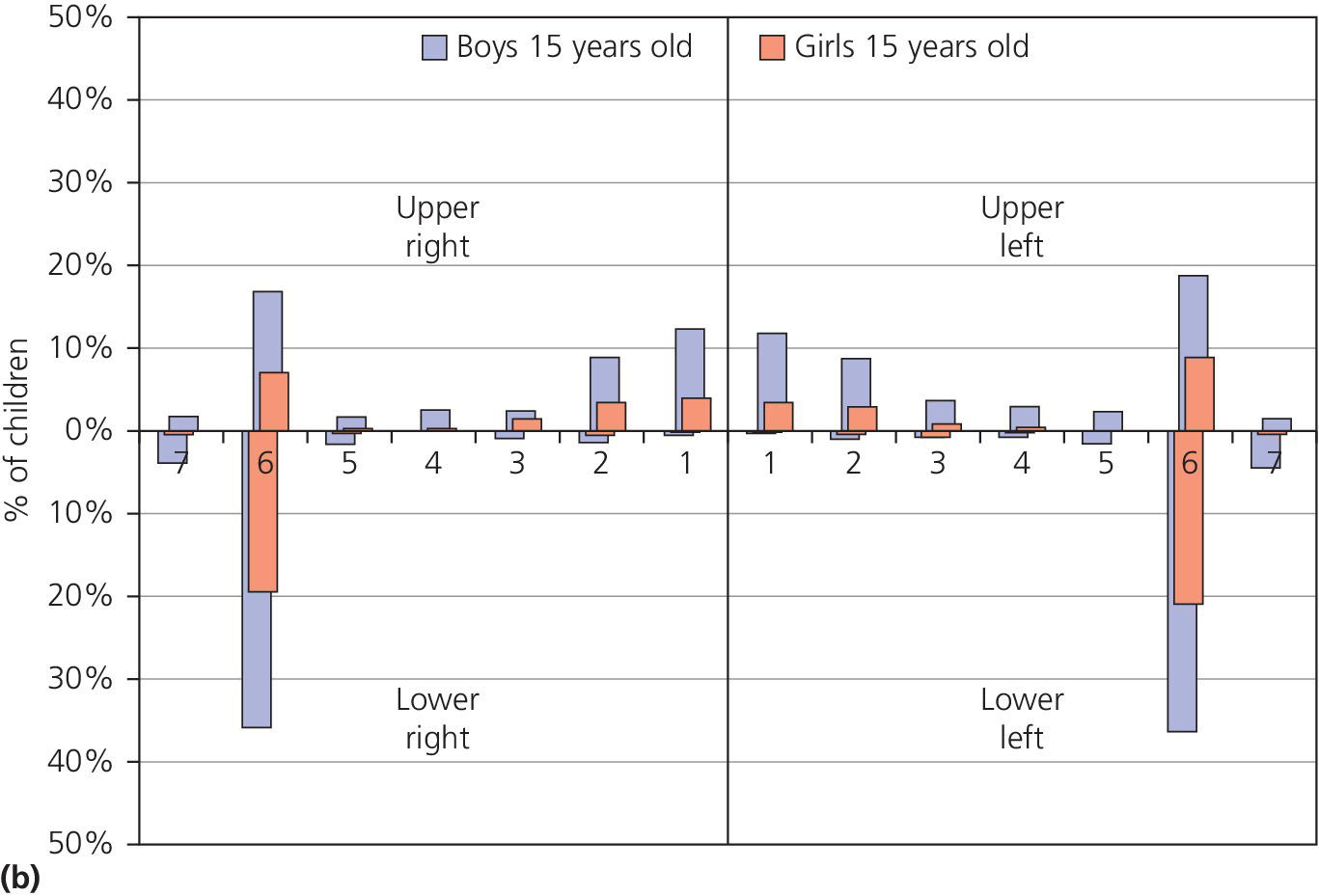
Figure 13.1 Distribution of dental erosion by tooth and by gender. Percentages of boys and girls with dental erosion by teeth at (a) 12 years of age and (b) at 15 years of age.
Source: Arnadottir et al. 2010 [46]. Reproduced with permission of John Wiley & Sons.
In severe cases of erosion in palatal surfaces of maxillary incisors a shoulder may be present cervically (Figure 13.2). Occasionally the approximal surfaces may also be affected. Cuppings (for explanation see second paragraph under heading “Clinical examination”) in the permanent dentition in children and adolescents are most commonly seen on the mandibular first molars, but can be found on all cusp tips or incisal edges (Figure 13.3). If erosion has been diagnosed on one tooth surface, it is important to examine other surfaces carefully for signs of tooth surface loss. This could, for example, be the presence of buccal–cervical defects or uprising restorations. Atypical localization of erosion exists and may be the result of, for instance, lemon sucking (Figure 13.4). Microhardness measurements have shown that deciduous enamel is softer than permanent enamel and that the progression of erosion is relatively more rapid than in permanent enamel. In addition, the fact that deciduous teeth are smaller in size further enhances the risk for complications by dental erosion [3]. (See Figure 13.5.)

Figure 13.2 Severe erosion on the palatal surface of the upper incisors. The enamel close to the gingival margin is intact and a shoulder is shown.
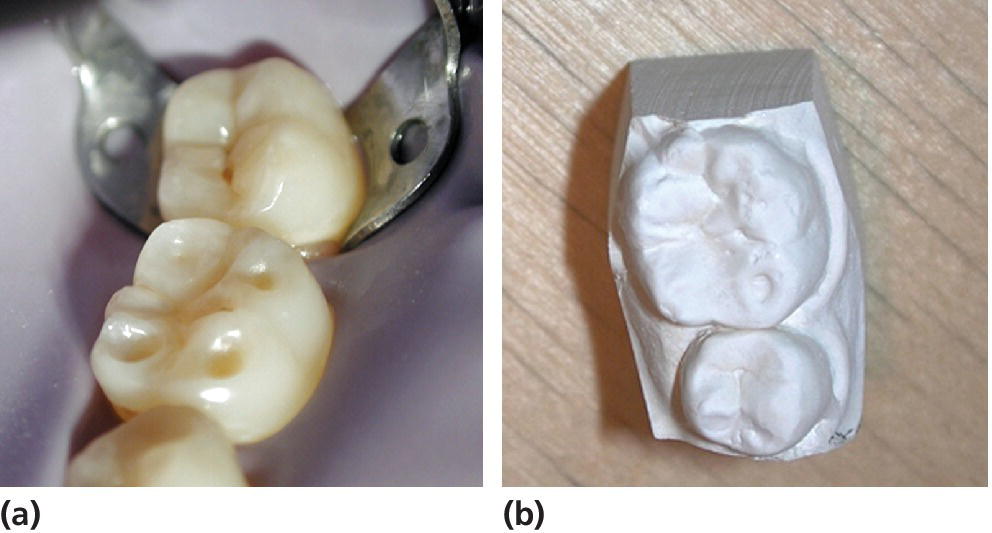
Figure 13.3 (a) Cuppings on a permanent first lower molar (tooth 36) in a young teenager. (b) Study cast from the same case.

Figure 13.4 Dental erosion as a result of lemon sucking in a 6‐year‐old child. Dental erosion has caused severe endodontic problem especially in region 52 and 51.

Figure 13.5 Near to pulp exposure on the palatal surfaces of anterior primary teeth. Secondary and tertiary dentin are shown.
Etiology
Traditionally, the etiologic factors for dental erosion have been divided into those of extrinsic and intrinsic origin (Box 13.2). The term “idiopathic erosion” has been used in cases of unknown etiology, but its clinical application is limited [4].
Examples of factors of extrinsic origins are all acidic drinks, and also acidic foods such as fruits and pickles, acidic medicines (e.g., acetylsalicylic acid and vitamin C tablets), and environmental exposure, such as highly chlorinated swimming pools.
The most common etiologic factor for dental erosion in children is high consumption of soft drinks, including fizzy drinks and fruit juices, which expose the dentition to frequent contacts with citric, phosphoric or malic acids. pH for some risk products are shown in Box 13.3.
Intrinsic factors include various gastrointestinal and eating disorders, e.g., vomiting, regurgitation, and rumination in which hydrochloric acid from the stomach comes into contact with the teeth.
Several chronic health conditions have been associated with dental erosion, especially those related to gastric acid/stomach disturbances and those affecting salivary secretion.
Factors decisive for erosive potential
The erosive potential of dietary components is estimated by measurements of initial pH, neutralizable acidity and ability to dissolve enamel in in vitro studies without the physiologic effects of saliva or frictional effects of the tongue. Besides the acidic challenges the content of calcium and phosphate in the products are important factors for the erosive potential and the dissolutions of tooth substance. Even at a very low pH it is therefore possible to prevent dental erosion in some drinks and milk products such as yogurt.
The interplay between these factors is often difficult to assess with regard to the overall risk and the clinical outcome.
Gastroesophageal reflux (disease)
Studies have shown that children with gastroesophageal reflux (disease) [GER(D)] have a higher prevalence of dental erosion compared to healthy children albeit it is considered to be a normal physiologic condition among infants. In the younger child, the symptoms will be diffuse and frequently described merely as stomach pain or persistent coughing. Symptoms in the older child have a more precise symptomatology: pain from the upper part of the stomach, heartburn, regurgitation, dysphagia, and coughing, especially at nighttime, are examples. In some cases, the patient does not present any typical symptoms at all; this is referred to as “silent reflux.” However, this condition may be detected by 24‐h pH monitoring, which is the gold standard in GER(D) diagnosis. In rare cases, reflux can be voluntary, which is called “rumination,” and most often found in connection with disabilities or eating disorders.
Asthma
Asthmatic problems are common in the child population and many asthmatic children have GER(D). While some reports have shown an increased prevalence of dental erosion in children with asthma others have not. In an asthmatic patient, bronchodilating medication may reduce salivary secretion and relax the lower esophageal sphincter with an increased potential for acidic reflux [5]. In addition, the medication itself may be acidic and mouth breathing resulting in dryness of the mouth is common, all of which raises the risk of dental erosion.
Eating disorders
Children and adolescents with eating disorders have an increased risk for erosion. In one study dental erosion was more than eight times more common in patients with eating disorders compared to controls. Self‐induced vomiting is seen in patients with bulimia nervosa, but also occurs in patients with other types of eating disorders; anorexia nervosa for example. Besides this, a high intake of sugar‐free soft drinks and fruits, excessive oral hygiene often combined with gastrointestinal disturbances, and salivary impairment are frequent among patients with eating disorders and raise the risk of erosion [6,7].
A large number of medications cause a dry mouth, e.g., anticholinergic drugs, medicines for GER(D), and psychiatric disorders. Cancer therapy with cytostatics or radiation treatment (often combined with vomiting) frequently compromises the function of the salivary glands and increases the risk for erosion. Diabetes (both types 1 and 2), hypoparathyroidism and hyperparathyroidism, hyperthyroidism, and congenital agenesis of salivary glands, Down syndrome, cerebral palsy, Prader‐Willi syndrome or the use of methylenedioxymethamphetamine (ecstasy) are other conditions associated with dental erosion [8].
Other factors associated with dental erosion
Drinking habits
An individual’s method of drinking acidic drinks plays an important role in the development of erosive lesions. The erosion damage is likely to be greater in those individuals who retain the drink in their mouth for some time before swallowing, compared to those who do not, as the contact time between the acid and the teeth is increased [9]. In a study, 43% of children with dental erosion were found to have a drinking habit such as swishing or holding compared to 3% in caries‐free and 15% in caries‐active controls [10], and in another study it was shown that the intraoral pH after drinking soft drinks differed between those with dental erosion and controls [11]. Dental erosion has also been associated with the consumption of acidic drinks in a baby’s bottle at bedtime or naptime [12]. Sucking through a straw may reduce the erosive potential of the drink if the straw is positioned towards the back of the mouth, which may be very difficult, especially for a child [13] (Figure 13.6).
Figure 13.6 pH decrease (mean values) for three methods of drinking and nipping from a baby’s bottle using the microtouch method and Cola Light. Holding = holding the drink in the mouth for 2 min. Long sipping = sipping from a glass for 15 min. Gulping = swallowing quickly three times over 5‐min intervals. Baby bottle = nipping from a baby’s feeding bottle for 15 min.
Source: Johansson et al. 2004 [9]. Reproduced with permission of John Wiley & Sons.
Salivary factors
An increased erosive action may be expected if the salivary secretion rate and buffering capacity are reduced. Saliva is important in the prevention of erosions through dilution and clearance of acidic products, and plays an important role in pellicle formation and demineralization and remineralization. It has been stressed that salivary characteristics may represent a risk for developing dental erosion lesions. The thickness of the pellicle varies between individuals and between different locations in the mouth, and may be reduced by acidic challenges such as soft drinks. A thicker pellicle provides more protection than a thinner one, and it has been suggested that salivary secretion and pellicle thickness strongly influence the location and development of erosion [14–16]. When measuring unstimulated and stimulated salivary flow rates, buffering capacity, and number of mutans streptococci in three groups of children, one with extensive erosions, one without caries, and one with high caries prevalence, the following were found: the erosion group showed great similarities concerning caries with the caries‐free group and great similarities concerning saliva characteristics with the high caries group [17]. Similar results were found in another study where children with erosion showed lower unstimulated and stimulated salivary rates, lower buffering capacity, and lower salivary pH, and a larger maximum pH drop after consumption of soft drinks compared to children without both erosion and caries [18] (Box 13.2).
Oral hygiene practices
It has been shown that individuals with erosion have better oral hygiene than those without erosion [19]. The modern practice of cleaning teeth is certainly more erosion conducive than a more irregular, less methodical, and less vigorous method of oral hygiene, since the erosive lesion develops on surfaces free of plaque. A plaque‐free surface could be a result of oral hygiene activities, but also a consequence of natural cleaning from the lips, tongue, and cheeks. Approximal surfaces are seldom free of plaque and this may be the reason why they rarely develop erosive lesions.
Oral hygiene activity, after an acidic challenge on the tooth surface, has been discussed but might result in a larger loss of tooth substance due to its being “presoftened” by acids. It has therefore been suggested to delay toothbrushing for at least an hour after the acidic challenge.
Lifestyle
The view has been expressed that “the lifestyle of today seems to increase the acidic challenge to the dentition and thereby introduces a new risk factor for the dentition” [20]. Lifestyle has a large impact on both general and oral health. It varies over time and often reflects social circumstances including dietary habits, physical activity, drug usage, and stress‐related factors. Important changes in the modern lifestyle are the increase in soft‐drink consumption, the decrease in milk consumption, and reduced physical activity in association with an increasing prevalence of obesity, diabetes, osteoporosis, and being overweight in the child population [21–24].
The fact that most soft drinks are consumed by young children and adolescents [25] especially increases the risk of dental erosion in these groups. Adolescents who frequently consume sport drinks during and after exercise when salivary secretion is lowered [15], as well as the young computer user who stays awake at night with the help of a cola drink, will have an increased risk of dental erosion.
A healthy lifestyle may also have an impact on the occurrence and severity of dental erosion, e.g., vegetarianism and dieting practices which are common among vegetarian children and adolescents. Vegetarians and children on a diet often have a high consumption of juices, fruits, and vegetables, perhaps with an added vinegar dressing, and in order to be orally healthy they also perform very thorough tooth hygiene.
Another recent lifestyle trend, especially among girls, is an increasing, unhealthy fixation on body shape and appearance. This may cause psycho‐pathological behavior leading for example to anorexia and/or bulimia including starving, vomiting, and a food pattern promoting dental erosion. These severe cases should be treated by a physician and at the same time by a dentist to ensure that the dental erosions do not aggravate [7].
The occurrence of dental erosion does not follow any obvious socioeconomic pattern. While some reports show that erosive wear is more common in children and adolescents with low socioeconomic status, other reports demonstrate the reverse. The same applies to gender differences, but in general it seems that boys are more affected than girls, which could be explained by the fact that boys generally drink more soft drinks compared to girls of a similar age.
The consequences of a new lifestyle often become obvious only when it is firmly established and it is difficult to revert to earlier routines. Thus, the oral medical aspects of dental erosion involve not only a proper dietary and medical history, but also knowledge of the person’s lifestyle. For example, it has been shown that the number of times per week children drink soft drinks relates to the number of teeth with dental erosion (Figure 13.7) [26].
Figure 13.7 Dose‐response relationship between frequency of soft drink intake and number of teeth affected by dental erosion in 7th grade (12 year‐old) and 10th grade (15 year‐old) children.
Source: Arnadottir et al. 2008 [26]. Reproduced with permission of Icelandic Dental Journal.
Case history and clinical examination
Case history
Children and adolescents are exposed to many different erosive challenges which may result in initiation or aggravation of already present dental erosion lesions. Taking a case history in patients with dental erosion is therefore often both extensive and time consuming. In younger children, where the case history has to be obtained from the parents, the dentist should recognize that not all parents are fully aware of their children’s dietary and drinking habits. Information about general health, e.g., gastric conditions, eating disorders, and asthma, including the type of medication, is relevant. Besides the obvious need for a dietary history, with special reference to acidic intakes including consumption of acidic drinks and fruits, other lifestyle factors which may be associated with an increase of exposure to erosive agents also need to be addressed. These include sports activities, computer use, and oral hygiene habits, for example. A dietary history should be performed over several days, preferably a week in order to include the weekend. This can, of course, be difficult especially in younger children, who besides their own family may meet different persons during the day in daycare centers and schools as well as when being with friends or grandparents. Consideration needs not only to be given to when and to what exposure, but also in what way, such as the method of drinking. Information on oral hygiene habits should be obtained. Finally, it is important to remember that an erosive lesion may not be the result of the child’s present habits, but could be caused by earlier exposure to an erosive challenge such as a previous period of high consumption of soft drinks. Some practical steps in taking a case history and in the clinical assessment of dental erosion are listed in Box 13.4.

VIDEdental - Online dental courses


