Chapter 13
Biopsy Techniques and Management of Intra-oral Calculi
Aim
This chapter describes biopsy techniques and the removal of salivary calculi.
Outcome
After reading this chapter you should understand the principles of biopsy and salivary calculus removal.
Biopsy Techniques
Prior to undertaking any form of biopsy a thorough history and examination should be carried out. This may provide a clue as to the nature of the lesion. When dealing with intra-oral lesions special attention should be paid to the smoking and alcohol history, together with details of any parafunctional habits.
A biopsy is a means of providing a specimen of tissue that is then subjected to histopathological examination. These are listed in Table 13-1.
| Biopsy techniques |
| Excisional biopsy (whole of lesion removed)
Incisional biopsy (part of lesion removed) Curettings Punch biopsy Fine needle aspiration biopsy Brush biopsy |
Biopsies may be performed in dental practice. It is important to stress, however, that if a lesion is suspected of being a malignancy the patient should be referred as a matter of urgency to a specialist oral and maxillofacial surgery unit (Fig 13-1). Lesions that appear malignant should not be biopsied in the general practice setting. One reason for this is that the exact location and dimensions of the lesion may not be apparent to the team that is eventually going to treat the patient. The two principal methods of biopsy used in general practice are the incisional and excisional types. Both procedures may be carried out under local anaesthesia. Lesions in inaccessible areas such as the posterior soft palate or back of tongue may require general anaesthesia and thus referral to a specialist unit. When injecting local anaesthetic prior to the biopsy it is important not to inject into the area that is being removed. This is to prevent tissue distortion by the injected solution.

Fig 13-1 This floor of mouth lesion is highly suspicious of a malignancy. Biopsy of such lesions is contraindicated in general dental practice. Urgent referral to a maxillofacial surgeon is the appropriate treatment.
Surgical Techniques
Incisional and excisional biopsies are carried out using sharp dissection so that any crush artefact of the specimen is minimised. Crushing of the specimen may render it useless for a histological diagnosis and necessitate a further surgical procedure for the patient. If instruments such as toothed forceps hold the specimen then these should be used at the periphery of the sample. This avoids crushing the main area of interest. The preferred method of preventing crushing is to use a suture to hold the specimen (Fig 13-2). The suture should be inserted before using the scalpel. The suture can be used to hold the specimen during removal and transfer to the transport container. Another advantage of inserting a suture is that it can be used to orientate the sample. Indeed, for large specimens a suture placed through one end is recommended. Informing the pathologist of the position of the suture enables orientation. If the suture is lost during transfer this should be mentioned in the pathology request form, as it may confuse diagnosis. The needle should be removed from the end of the suture prior to transfer to the laboratory to avoid needle-stick injury.
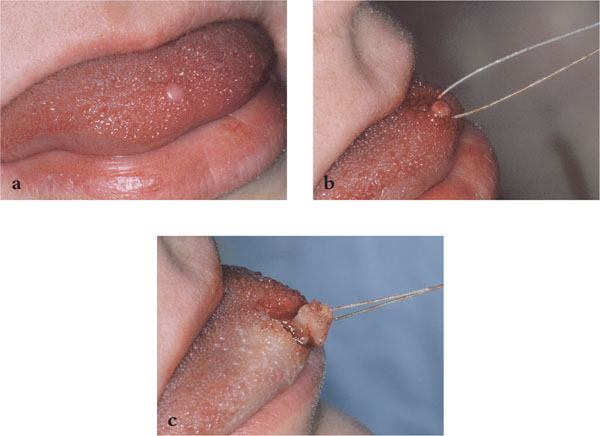
Fig 13-2 Use of a suture to hold a biopsy specimen. (a) The lesion for biopsy on the tip of the tongue. (b) A suture passed below the lesion. (c) The specimen is held by the suture preventing crushing of the sample.
In excisional biopsies the whole lesion is removed (Fig 13-3). The technique is suitable for small lesions that appear clinically benign, such as papillomas or polyps. When removing a mucocele (Fig 13-4), any normal minor salivary glands noted in the surgical field should be excised, as these may have been traumatised during the surgery. Any damaged glands that remain may produce a further mucocele. When performing an excisional biopsy, an elliptical incision is normally used. The longer dimension should be parallel to important structures to avoid damage (see below). When excising benign lesions, a 1–2 mm margin of normal tissue is included.
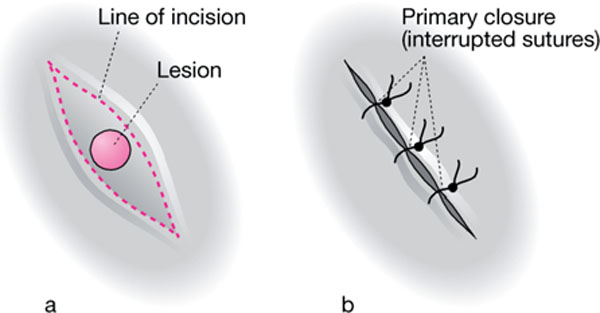
Fig 13-3 The technique of excisional biopsy.

Fig 13-4 When removing mucoceles any surrounding minor salivary glands included in the surgical site should be included.
With incisional biopsies, the whole lesion is not removed, but a clinically representative sample is taken in order to facilitate diagnosis and therefore provide a basis for appropriate subsequent treatment (Fig 13-5). Elliptical incisions are recommended. An important factor that determines the position of an incisional biopsy of a large lesion is the position of other important structures. Areas close to the parotid and submandibular ducts and neurovascular bundles such as the mental, lingual and greater palatine nerves should be avoided. Incisional biopsy may be used to diagnosis the nature of mucosal lesions, such as red and white patches. A non-healing ulcer should also be biopsied in this way. A morphologically normal piece of tissue should be removed in continuity with the lesion to show the pathologist the junction between the two. When performing an incisional biopsy in a suspected vesiculo-bullous disorder, it is important not to sample an ulcerated lesion (Fig 13-6). The presence of epithelium is important if immunofluo/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


