11
Patients with Periodontal Problems
Prevalence of periodontal disease
Malocclusion and periodontal disease
Orthodontics and periodontal disease
Indications for orthodontic treatment in periodontally involved patients
Treatment of patients with flared and extruded upper incisors
Tissue reaction to intrusion of teeth with horizontal bone loss
Treatment of patients with vertical bone defects
What are the periodontal limits for orthodontic tooth movement?
Sagittal movement
Transverse movement
Sequence of treatment in periodontally involved patients
Conclusion regarding Influence of orthodontic treatment on periodontal status
References
Prevalence of Periodontal Disease
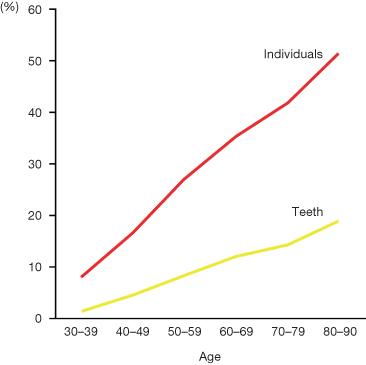
Periodontal problems contribute to the development of malocclusion in a substantial number of adult orthodontic patients. Indeed, as is commonly seen in the Western world, the risk of gingival recessions, attachment loss and probing depth >4 mm increases significantly with age (Hugoson et al. 1995; Albandar 2002a,b) (Fig.11.1). Both general and local factors have been described as influencing the development of periodontal disease (Table 11.1).
Table 11.1 Factors influencing the development of periodontal disease
| General factors | Local factors |
| Gender | Oral hygiene |
| Genetic factors | Untreated dental caries |
| Social status | Dental restorations |
| General health | Microbiological factors |
| Host immune factors | Crowding |
| Smoking | Occlusion |
Fig. 11.1 Increase in the loss of periodontal support in relation to age.
(Redrawn from Albander (2002b), with permission.)
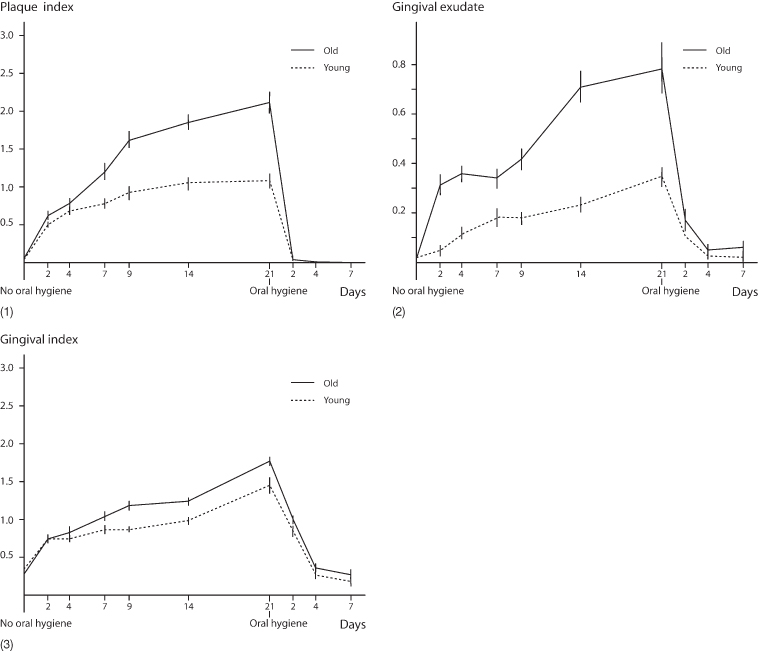
The periodontal condition is crucial when considering orthodontic treatment in older adults. This is not the case in adolescent or young adults where the correlation between gingivitis and periodontitis is only weak. Shei et al. (1959) found that with increasing age, oral hygiene had a significantly greater impact on the marginal bone level (Fig 11.2). This was confirmed by a study in which students below 25 years of age and teachers above 40 years were compared following a 21-day period of oral hygiene abstention. The older group not only accumulated more plaque but also developed gingivitis more rapidly than the young individuals (Fig 11.3) (Holm-Pedersen et al. 1975).
Fig. 11.2 (1–5) Relati onship between oral hygiene and marginal bone level at different ages. It is obvious that the relation between oral hygiene and marginal bone level becomes more significant with increasing age.
(Redrawn from Shei O, Waerhaug J, Lovdal A and Arnulf A (1959) Alveolar bone loss as related to oral hygiene and age. J Periodontol 26, 7–16.)
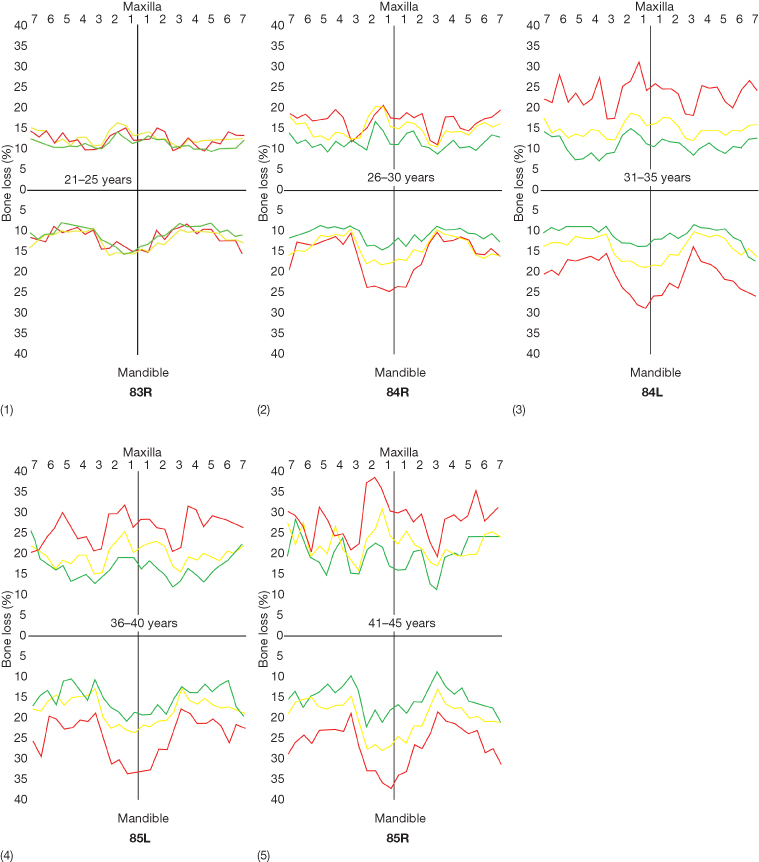
Fig. 11.3 Influence of absence of oral hygiene in young and older adults. The figure illustrates the consequences of abstention from oral hygiene for 3 weeks. Both plaque accumulation (1) and inflammation manifested as gingival exudate (2) and gingival index (3) were greater in the older than in the young probands.
(Redrawn from Holm Pedersen P, Agerbaek N and Theilade E (1975) Experimental gingivitis in young and elderly individuals. J Clin Periodontol 2, 14–24, with permission.)
Malocclusion and Periodontal Disease
A malocclusion has no direct influence on periodontal breakdown (Geiger et al. 1972; Shaw et al. 1980). However, it has been indicated that untreated occlusal discrepancies are associated with more rapid progression of periodontal disease and that occlusal treatment reduces the progression (Harrel and Nunn 2001; Reichswage and Rydesky 2002). Several studies propose that certain malocclusion traits can be considered risk factors due to the strong correlation between them and aspects of periodontal disease, for example pocketing and crowding, (el-Mangoury et al. 1987; Staufer and Landmesser 2004); bone level and crowding (Jensen and Solow 1989) and bone loss and tooth rotation (Peretz and Machtei 1996). The relationship between periodontal disease and crowding is most likely indirect since several studies have demonstrated that plaque accumulation is more pronounced in crowded areas (Ingervall et al. 1977; Buckley 1981). In addition, Chung et al. (2000) demonstrated an increased number of periopathogenic species such as spirochaetes, motile rods, Fusobacterium species, Capnocytophaga species, Campylobacter rectus and Peptostreptococcus micros in crowded compared with non-crowded areas. Diedrich (2000) also points to the relevance of crowding, not only with respect to plaque retention but also with respect to the altered topography of the gingiva and the alveolar bone. To limit the effect of crowding on the periodontium, Helm and Petersen (1989) stated that the special topography of the crowded areas call for special professional efforts of hygiene education and therapy.
The relationship between crowding and periodontitis does work both ways as the migration of anterior teeth occurs more frequently in the presence of periodontal disease, leading to more crowding in the lower arch, which then makes it more difficult to maintain a healthy periodontium (Towfighi et al. 1997). The only malocclusion in which there is a direct correlation between malocclusion and attachment loss is a deep bite impinging either lingually to the upper incisors or/and labially to the lower incisors (Sanavi et al. 1998) (Fig 11.4). Another way in which occlusion leads to periodontal disease may be via the distribution of occlusal forces. It has also been demonstrated repeatedly (Ericsson and Lindhe 1982, 1984; Svanberg et al. 1995) that although jiggling forces from occlusal trauma do not in themselves produce loss of connective tissue attachment if the periodontium is healthy, jiggling will, in the presence of periodontitis, accelerate the loss of attachment (Burgett 1995).
Fig. 11.4 (1) Patient with a deep bite and impingement lingual to the upper incisors (2), and trauma to the gingiva labial to the lower incisors (3).

The indirect effect of traumatic occlusion may be explained by the fact that it frequently results in the loosening of the teeth, which has been shown to be a risk factor as the prevalence of specific periodontopathogens increases and thereby leads to a more rapid breakdown of the attachment (Grant et al. 1995; Melsen et al. 1998). Increased mobility is conversely also seen in relation to orthodontic treatment whereby the treatment in itself constitutes a risk factor if the periodontal health is not completely under control.
Orthodontics and Periodontal Disease
Adult orthodontics and periodontal disease have been the focus of increasing attention over the past 25 years. Miethke and Melsen (1993) searched the literature, from between 1984 and 1993, using the keywords adult orthodontics and periodontal disease and found 104 papers. Thirty-one were case reports, 24 longitudinal and 9 cross-sectional studies. A similar search done with the same keywords between 1994 and 2003 disclosed 261 papers (Table 11.2).
Table 11.2 Papers with the keywords adult orthodontics and periodontal disease
| 1984–1993 | 1994–2003 | |
| Total number | 104 | 261 |
| Case report | 31 | 116 |
| Clinical trial | 33 | 24 |
| Technique described | 20 | 85 |
| Case–control study | 1 | 8 |
| Review | 19 | 28 |
Most patients ask for orthodontic treatment in anticipation that it will improve both the aesthetics and overall prognosis of the dentition. However, patients should be informed that orthodontic treatment in itself cannot be considered protective in relation to further development of periodontitis.
The influence of orthodontic treatment on the periodontium has been described as both beneficial and detrimental. Zachrisson and collaborators showed that orthodontics can contribute to the development of the loss of attachment especially in relation to space closure following extraction (Sjolien and Zachrisson 1973; Zachrisson and Alnaes 1973). The beneficial impact of the treatment result on the oral hygiene, might, on the other hand, explain that when the same authors performed a longitudinal study on 38 children (Alstad and Zachrisson 1979), they found that the treated patients seemed to maintain better hygiene following treatment even than the control group.
However, the detrimental effect of orthodontic treatment in the absence of an adequate oral hygiene programme has been shown both in papers describing iatrogenic damages and in animal experiments. It has been invariably found that moving a tooth into an infected infrabony defect will enhance the destruction of connective tissue attachment (Ericsson and Thilander 1978; Wennström et al. 1993). The experiments were carried out on dogs with experimentally induced periodontal disease. The periodontium of adult patients with periodontal disease can be expected to react even less favourably, since their resistance can be anticipated to be less than that of the dogs in which the disease was provoked.
Iatrogenic damage in orthodontics seems to be age dependent, rendering the orthodontic treatment of older adults even more risky. When the periodontal status of young adults who had received orthodontic treatment at least 10 years earlier was compared with that of adults with untreated malocclusions no differences were found in any of the periodontal variables including plaque inflammation, bleeding on probing pockets depth, recessions, loss of attachment and crestal bone level (Polson et al. 1988). Conversely, Lupi et al. (1996) studied 88 adult patients who had had orthodontic treatment and found that the percentage of patients with loss of alveolar height exceeding 2 mm from the cementoenamel junction to the alveolar crest increased during treatment from 19% to 37%. However, in this study, there was no information about the hygiene of the individuals. The importance of good oral hygiene was stressed both by Eliasson et al. (1982) and Boyd et al. (1989) who both found that when periodontal health was maintained during treatment, orthodontics had no iatrogenic effects and might even be beneficial.
Vanarsdall (1995) on the other hand, addressed oral hygiene from a more pragmatic aspect, stating that not all patients can be expected to comply with the recommended maintenance schedule. He still recommended to compromise treatment that may reduce the chances of a reinfection following adequate periodontal treatment.
Indications for Orthodontic Treatment in Periodontally Involved Patients
Before starting treatment, several questions could be posed:
- What are the characteristics of patients with periodontal disease seeking orthodontic treatment?
- Who can realistically benefit from orthodontic treatment?
Patients’ concern for their teeth is more closely related to the perceived need for treatment rather than to the objective need judged by the orthodontist (Tervonen and Knuuttila 1988; Lundegren et al. 2004). The patient will seek treatment when he or she no longer finds their dentition acceptable. Most patients with periodontal breakdown have experienced migration of teeth in relation to the development of their disease (Fig. 11.5). It is, however, important to determine whether the periodontal disease and the development of the malocclusion is a slowly developing process or whether the patients can relate the migration of the teeth to any specific change in the local or general environment.
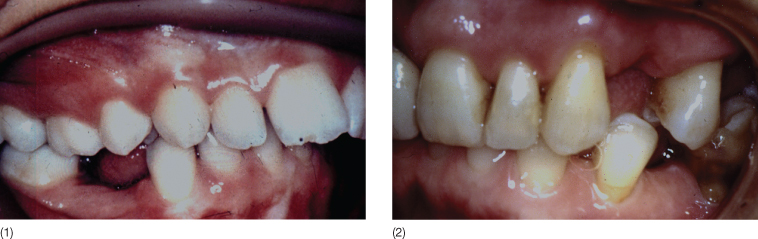
Fig. 11.5 (1–4) Pre-treatment photographs of a patient whose need for orthodontic treatment became evident following the periodontal surgery that had led to opening of spaces and ‘black’ spaces between the incisors. She now felt that she was pressing the tongue against the spaces when speaking and that she was starting to lisp. (5–8) Following orthodontic treatment with intrusion and retraction of the upper incisors. Note the shortening of the clinical crowns.

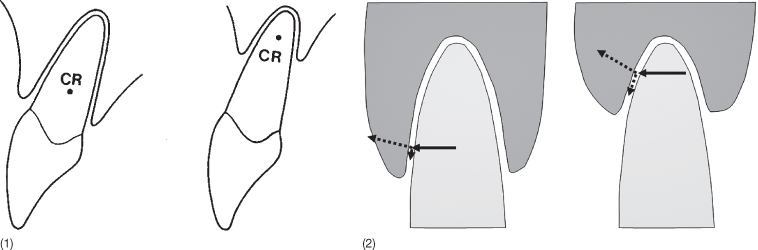
Tooth migrations leading to unacceptable malocclusions are closely related to change in the marginal bone level. This can be caused by periodontitis (Hugoson et al. 1998; Albandar and Rams 2002) but can also be an adverse effect of a toothbrushing habit (Pattison 1983; Spieler 1996; Smukler and Landsberg 1984; Litonjua et al. 2003). With changes in the marginal bone level, the centre of resistance is displaced apically, whereby occlusal forces on the incisors will lead to tipping and extrusion, as the horizontal forces acting on the oblique alveolar wall will lead to shearing. Thereby a vicious circle commences, consisting of further migration and shearing forces (Fig. 11.6).
Fig. 11.6 (1) Effect of marginal bone loss on the location of the centre of resistance (CR). (2) When the tooth is submitted to a horizontal force, this is converted to a shearing force in the periodontal ligament leading to relative extrusion. The more oblique the surface, the more is the shearing force leading to extrusion.
The most common symptoms of malocclusion in patients with periodontal disease are deepening of the bite, increased overjet and development of spacing between the upper incisors and lower incisor crowding. In the incisor region, general flaring is typically seen, but extrusion of single teeth with local periodontal disease may occur (Diedrich 1999). This is often seen in relation to the upper lateral incisors and has been attributed to the particular anatomy of these teeth. A fissure on the lingual aspect of these teeth as a result of an invagination, sometimes referred to as dens in dente, allows for the development of inflammation leading to localized bone loss due to the increased intra-periodontal pressure, which secondarily can lead to extrusion of the involved teeth (Chen et al. 1990; Fristad and Molven 1998) (Fig. 11.7). When flaring starts to occur, it may influence the balance between the internal and the external muscle matrices. Once the lower lip is positioned behind the upper incisors during swallowing and/or speech or para-function, it can lead to rapid deterioration of the dentition or aggravation of the malocclusion. Increase in overjet may also occur as a result of collapse due to loss of posterior teeth (Fig. 11.8). For most patients, impaired aesthetics is the reason for seeking treatment.
Fig. 11.7 (1) Personal photograph taken when the patient was around 20 years of age. Note that the maxillary lateral incisors are shorter than the central incisors. (2,3) Twenty-six years later, the lateral incisors appear longer than the central incisors. These teeth have extruded due to periodontal disease. The periodontium is healthy following periodontal surgery but the occlusion is not satisfactory. (4,5) Following orthodontic treatment, a nice smile was re-established.

Fig. 11.8 (1, 2) Intraoral photographs of a patient in whom loss of posterior teeth led to a deepening of the bite due to posterior tipping of the anterior teeth.
So can all patients with periodontal disease and malocclusions benefit from orthodontic treatment? Before planning orthodontic treatment in patients with periodontal disease it should be ascertained that the patient will be willing to go through the necessary periodontal preparation and is able to maintain a healthy but, in their case, reduced periodontium. Even so, it should be born in mind that patients with a history of earlier periodontal disease are high-risk patients (Loe and Morrison 1986). Patients who have developed a secondary malocclusion or in whom there is aggravation of an existing malocclusion in relation to periodontal breakdown, however, cannot be treated to a satisfactory result by periodontal and prosthodontic treatment without involving orthodontics. Loading of the spontaneously migrated teeth during normal function will often be detrimental and migration will continue in spite of a healthy periodontium. Solving the problem by prosthetic rehabilitation alone is rarely advisable as the patient’s aesthetic needs can seldom be fulfilled. The majority of patients will therefore benefit from orthodontic treatment that re-establishes a functional equilibrium, if possible, or create an occlusion that allows for satisfactory rehabilitation.
Malocclusions in adult patients that may be considered as indications for orthodontic treatment are:
- Intra-arch problems, anomalies that interfere with maintenance of optimal oral hygiene or necessary replacement of missing teeth
- Inter-arch problems, deviations in occlusion that do not allow normal function
- Functional deviations, malocclusions related to forced bites
In many patients, the problems fit into more than one category:
- Intra-arch problems include: adverse gingival topography, poor crown to root ratio, uneven bone level, osseous defects, diastema (flaring), excessive root proximity, crowding, tipping and rotation, poor distribution of the existing teeth.
- Inter-arch problems comprise: sagittally, increased overjet or inversion; vertically: both deep and open bite; transversely: crossbite and scissor bite.
- Signs of malfunction that may contribute to aggravation of a malocclusion include flared incisors with lip catch, posterior and lateral forced bite reflected in abnormal wear of teeth.
The treatment goal for orthodontic treatment in such patients is to establish an occlusion that allows optimization of the necessary oral rehabilitation and maintenance. In addition, the treatment should aim for an aesthetically satisfactory result, thus taking the patient’s chief complaint into consideration.
The tooth movements required in periodontally involved patients include sagittal and transverse movements to relieve crowding, uprighting of teeth tilted into extraction spaces and intrusion, often combined with retraction or protraction and closure of diastema. When attempting to move teeth horizontally, it should be appreciated that the bone loss results in an apical displacement of the centre of resistance and that the moment-to-force ratio therefore has to be adjusted to the individual situation (Fig. 11.6).
Treatment of Patients with Flared and Extruded Upper Incisors
Correction of flared anterior teeth in patients with horizontal bone loss as a result of combined proclination and extrusion of these teeth involves a combination of retraction and intrusion. Mere retroclination of the flared teeth would lead to a deepening of the bite. Melsen et al. (1989) studied the effect of intrusion on the periodontium in the patients with horizontal bone loss in 30 consecutive patients (5 men and 25 women, aged 22–26 years) with deep bite and need for intrusion. In 24 patients the malocclusion had developed or worsened in relation to progressive periodontal disease and in six patients deepening of the bite had occurred following extraction of posterior teeth.
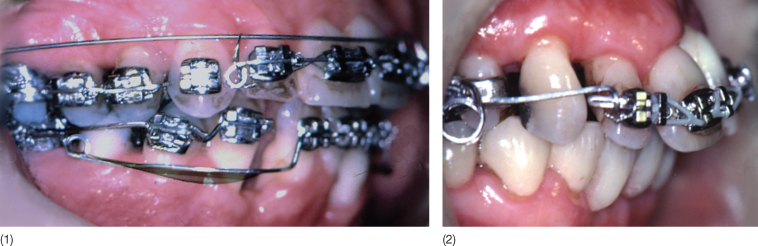
Before orthodontic treatment, all patients received conservative periodontal treatment including scaling and root planing and oral hygiene instruction. In addition, a modified Widman flap operation was necessary in 15 patients to reduce the pockets to the acceptable 3–4 mm or less (Fig. 11.9). An unavoidable and undesirable side effect of surgery was that the clinical crowns became longer. As the dentition had severely deteriorated, the patients were (partly as a joke) asked: ‘Do you want your incisors longer or no longer?’ All patients accepted orthodontic treatment. One week after surgery, active intrusion started using a segmented appliance approach. The anchorage unit comprised two rigid buccal segments including the available molars and premolars. These segments were connected across the palate with one or two 0.036 inch stainless steel transpalatal arches. A stiff stainless steel full-size segment consolidated the anterior teeth that had to be intruded and maybe retracted (Fig. 11.10). The active appliance consisted of a titanium molybdenum alloy (TMA) base arch or two cantilevers delivering an intrusive force of 5–20 g per tooth depending on the periodontal support. The point of force application and the configuration of the wire were chosen based on the estimated centre of resistance so that the desired combination of intrusion and proclination or retroclination could be generated (Dalstra and Melsen 1999). The appliance design is discussed in Chapter 7.
Fig. 11.9 A patient requesting treatment for flared upper incisors. (1) The pre-treatment photograph was taken after periodontal preparation leading to elongation of the clinical crowns. (2) The post-treatment photograph demonstrates the shortening of the clinical crowns as a result of intrusion of the extruded teeth.
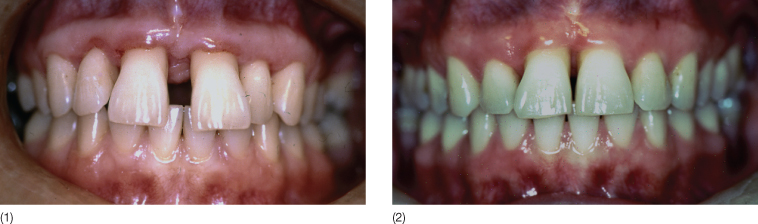
Fig. 11.10 Appliance used for intrusion. (1) A base arch made of 0.018 inch titanium molybdenum alloy (TMA). This was used when maximum intrusion and little retraction was required. (2) Three-piece mechanics used for combined retraction and intrusion.
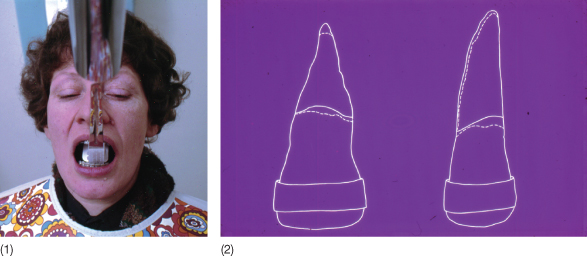
During the treatment, which lasted between 6 and 8 months, the patients received continuous periodontal follow-up, including instruction for home care and regular check-ups with the periodontologist. The changes occurring as a result of the treatment were evaluated on intraoral photographs, headfilms, periapical radiographs of the upper incisors, study casts, all taken at the start and end of the treatment. The alveolar bone level was evaluated on the periapical radiographs with the aid of a special film holder that ensured the reproducibility of the intraoral radiographs (Fig. 11.11). The peri-apical radiographs demonstrated a coronal displacement of the marginal bone level. Based on drawings of the superimposed intraoral radiographs, the changes occurring over treatment were calculated.
Fig. 11.11 (1) Special film holder allowing identical exposure of the individual tooth. (2) Tracing of the periapical radiographs indicating the marginal bone level before and after the intrusion. Slight apical resorption could also be verified in most cases.
The mean increase in the area of the osseous alveolus of 7% varied from a gain of 22% to a loss of 15% (Table 11.3). Nineteen of the 30 patients demonstrated improvement in alveolar support; five exhibited no change while five patients had lost bone, in two of these patients, this could be attributed to inadequate maintenance of oral hygiene and one patient had pronounced tongue pressure counteracting the retraction, for which reason the treatment resulted in a loosening of the incisors during retraction.
Table 11.3 Change in bone support area of alveolus (%)
| Mean | Minimum | Maximum |
| 6.76 | –1.5 | +22 |
The movement of the incisors was evaluated on the head films in relation to a coordinate system comprising of the hard palate as the X-axis and the perpendicular to the reference point pterygomaxillare as the Y-axis (Fig. 11.12). As all the patients were adults, these reference points were stable. A template of the central incisor was made for each patient and the best possible estimate of the centre of resistance, 40% from the marginal bone level was indicated on the templates. The templates were placed according to the best fit on the pre- and post-treatment head films. The vertical movement of the apex varied between 2 mm extrusion and 5 mm intrusion. Extrusion of the apex was seen when retroclined incisors were proclined in combination with intrusion of the crown (Table 11.4). The maximum intrusion of the apex occurred when proclined teeth were retroclined in combination with the intrusion. The intrusion of the centre of resistance varied between 0 and 4 mm while the displacement of the incisal edge was between 2 mm extrusion and 6 mm intrusion.
Table 11.4 True intrusion (mm)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


