CHAPTER 1
Introduction
• A symptom-based approach to diagnosis
• Special investigation of orofacial disease
• Salivary gland investigations

A symptom-based approach to diagnosis
A clinician’s assessment of a patient presenting with an oral symptom or sign of disease may be viewed in a manner similar to that of a detective attempting to solve a crime. On some occasions the solution is straightforward, based on a short history obtained from the patient and examination of the lesion. On other occasions the diagnosis may be more elusive and require the analysis of a more complicated history and a more extensive clinical examination. In addition, special tests, in particular hematological assessment, microbiological sampling, and tissue biopsy, are of invaluable help in establishing the definitive diagnosis.
The material in this book has been grouped on the basis of the principal clinical sign or symptom obtained from the history and clinical examination.
History
A diagnosis can only be achieved after a detailed history of the complaint has been obtained. In addition, a full medical and dental history should be taken. Specific information related to the orofacial complaint should include details of site, onset, and relieving and exacerbating factors. Further questioning often depends on the clinical signs observed but will usually include the following:
• First episode or recurrent problem? If recurrent, how many lesions and duration?
• Painful? If painful, nature, severity, timing, and duration?
Clinical examination
There is no ‘right’ or ‘wrong’ way to examine the orofacial tissues. However, it is essential to ensure that all areas and structures have been assessed in an organized and systematic fashion. Universal precautions should be followed throughout the examination including the wearing of gloves.
EXTRAORAL EXAMINATION
The clinical examination begins as soon as the patient presents in the clinic. Information on gait and the presence of any physical disability becomes evident as the patient gets into the examination chair. In the context of orofacial disease, the patient should be examined for obvious facial asymmetry and general appearance of the skin.
The lips should be examined for evidence of erythema and crusting, particularly at the angles. Any swelling within the lips should be palpated. The parotid gland should be palpated along with the cervical and neck lymph nodes. The sublingual and submandibular salivary glands should be palpated using a bi-manual technique (1). It may be necessary to assess the function of each of the cranial nerves.
INTRAORAL EXAMINATION
A good light source and dental mirror are required for examination of the intraoral structures. Initially, an overall assessment should be made, although it likely that a more detailed examination of particular areas will be required later depending on the signs and symptoms. The mucosa should appear moist and pink. Clear saliva should be present in the floor of the mouth.
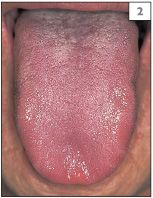
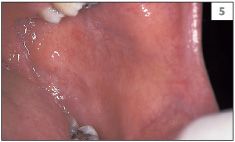
The teeth should be examined for evidence of gross caries, discoloration, and presence of plaque or calculus. Any relationship between the teeth or restorations and mucosal abnormalities should be noted. The entire oral mucosa should be examined, including the dorsum and the lateral margins of the tongue, the buccal and labial mucosae, the hard and soft palate, and the floor of the mouth (2–8).
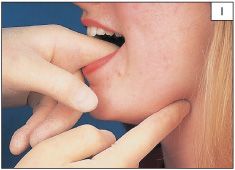
1 Bi-manual palpation of the left submandibular gland.

3 Left lateral margin of the tongue.

4 Right lateral margin of the tongue.



Normal structures
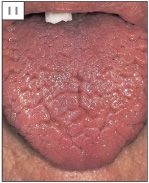
Normal structures within the mouth are sometimes mistaken for pathological conditions. Examples of this are the circumvallate papillae (9) and foliate papillae (10) of the tongue, fissured tongue (11), lingual varicosities (12, 13), and ectopic sebaceous glands (14).
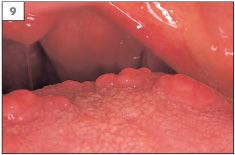
9 Circumvallate papillae at the junction of the anterior two-thirds and the posterior third of the tongue.
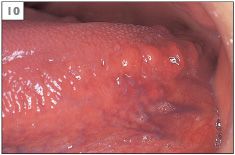
10 Foliate papillae on the posterior lateral margin of the tongue.



Special investigation of orofacial disease
The special investigations that are employed in oral medicine may be grouped under four headings: hematological, microbiological, tissue biopsy, and salivary gland investigations.
HEMATOLOGICAL ASSESSMENT
The range of hematological tests available to assist in the diagnosis of oral facial disease is large. Details of specific tests required for each condition presented in this book are given within the main text.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


