1
Clinical and Cephalometric Analysis
Introduction
Orthodontics is the area of dentistry concerned with the management of deviations from normal occlusion or malocclusion and involves treatment of children, adolescents and, increasingly, adults. Malocclusion is a variation on normal occlusion and is not a disease entity. Consequently, orthodontic planning and management does not involve binary decisions, but rather evaluation of a range of possibilities to decipher the most appropriate option for each individual.
An ideal static occlusion is characterized by class I molar and incisor relationships, with well-aligned teeth. An acceptable occlusion, however, develops naturally in only 30–40% of the population in Western societies. The occurrence of an acceptable occlusion is multi-factorial, although important factors include the size of the jaws; the relationship of the jaws to each other; the size, number and morphology of the teeth; and the morphology and behaviour of the lips, tongue and peri-oral musculature.
Given that malocclusion does not represent a pathological process but rather a variation from an accepted norm, there is little agreement, even among orthodontists, as to when orthodontic treatment becomes necessary (Richmond et al., 1984). As a consequence, a variety of orthodontic indices have been developed to ration treatment where care is provided as part of a public health service, such as in the UK and Scandinavia (Brook and Shaw, 1989), based primarily on aesthetic and dental health impairment.
The demand for orthodontic treatment has increased universally, particularly over the past two decades. A desire to enhance dental appearance is the underlying motivation for most patients who seek orthodontic treatment (Shaw et al., 1991). Furthermore, the lay public has developed an increasing awareness of the importance of the dentition to overall attractiveness. Carefully planned and well-executed orthodontics can also enhance facial appearance, which in turn has been linked to improved social skills, greater desirability, higher intellectual ability and enhanced occupational prospects (Shaw et al., 1979).
Deviation from occlusal norms may leave children susceptible to harassment, teasing and bullying, with obvious psychosocial implications (Shaw et al., 1980; Seehra et al., 2011). Consequently, orthodontic treatment may have significant psychosocial benefits (Shaw et al., 1980; O’Brien et al., 2003) and can often lead to improved oral health-related quality of life. Similarly, combined orthodontic–surgical treatment has been linked to notable enhancement of both self-esteem and quality of life (Arndt et al., 1986).
The undoubted benefits of orthondontics are, however, reliant on careful diagnosis, planning and management. Clinical assessment and radiographic analysis are central to the formulation of appropriate treatment decisions leading to the best aesthetic and functional outcome from treatment.
As in any other area of medicine or dentistry, to reach a diagnosis in orthodontics requires a thorough history, examination and special tests. A comprehensive history should be undertaken to clarify the motivation for treatment, the dental and orthodontic history, and any relevant medical history that might impact on the provision of orthodontic treatment (Patel et al., 2009).
Dental History
A history of dental attendance is relevant in relation to caries experience and the presence of restorations. Caries experience is the best predictor of future caries. Poor oral hygiene predisposes to two risks of treatment: gingivitis and demineralization. Premature loss of primary teeth due to caries may also have consequence for the developing dentition. In particular, early loss of primary teeth may hasten or retard eruption of permanent teeth and lead to space loss, which can result in centre line discrepancies or potential tooth impaction.
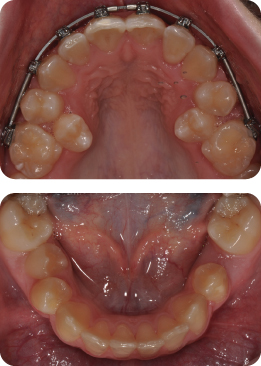
What Has Led to Crowding of the Second Premolars in Figure 1.1?
Early loss of the second primary molars has allowed the first permanent molars to drift forward in the dental arch. The second premolars are most vulnerable to space loss in this region.
Restorations
Heavily-restored teeth may pose problems in relation to bonding, necessitating alteration of the bonding protocol, with sandblasting of amalgam and precious metal restorations proven to enhance bond strength (Zachrisson et al., 1995; Büyükyilmaz et al., 1995). There is conflicting evidence in relation to the susceptibility of root canal-treated teeth to root resorption during treatment. Nevertheless, the health of root-treated teeth should be monitored throughout treatment.
Trauma
A history of trauma to the dentition should be investigated. Previously traumatized teeth risk loss of vitality irrespective of orthodontic treatment. This potential eventuality should be discussed at the outset as part of the informed consent process. In addition, traumatized teeth may also be at risk of undergoing more apical root resorption during treatment. The nature and timing of the traumatic injury has a bearing on further treatment (Kindelan et al., 2008) (Table 1.1).
Table 1.1 Timing of further treatment for traumatic injury
| Type of injury | Recommended observation period before orthodontic treatment |
| Fracture without pulpal involvement | 3 months |
| Subluxation | 3 months |
| Extrusive luxation | 3 months |
| Minor lateral luxation | 3 months |
| Moderate/severe lateral luxation | 1 year |
| Intrusion | 1 year |
| Avulsion | 1 year |
Previous Orthodontics
Increasingly, potential orthodontic patients, particularly adults, may have undergone previous treatment. Details of the original malocclusion may help to decipher the aetiology of both the presenting and residual malocclusion. Potential consequences of incomplete treatment include residual malalignment and spacing, traumatic overbite, residual overjet, crossbite and relapse. Previous failure to complete a course of orthodontic treatment may raise questions with respect to compliance (Murray, 1989). Where compliance is questionable, it may be inadvisable to embark on an ambitious course of orthodontic treatment.
Furthermore, contemporaneous records are important to reveal deleterious effects of the primary phase. Rarely, significant root resorption may limit the feasibility for retreatment.
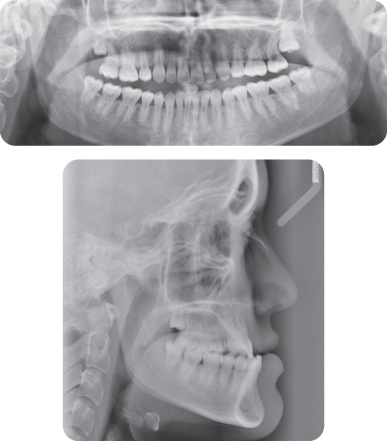
What Do You Notice with Respect to the Radiographic Appearance of the Maxillary Incisors (Figure 1.2)?
The maxillary incisors, particularly the UR1, UL1 and UR2, have experienced extensive root resorption during the first phase of treatment.
How Will This Finding Influence Further Management?
The patient is keen to undergo combined orthodontic–surgical treatment to address her malocclusion comprehensively. Prior to instituting such treatment, the patient will be counselled in relation to the likelihood of further resorption. If the patient opts to undergo combined treatment, attempts will be made to avoid an upper fixed appliance. If an appliance is to be placed, light forces will be applied, there will be a premium on excellent oral hygiene and the duration of treatment will be necessarily short with realistic objectives.
Family History
The contribution of genetic factors to malocclusion has been established in family and twin studies. Concordance of occlusal patterns in monozygotic twins provides support for the influence of genetics on malocclusion, while discordance between monozygotic twins suggests occlusal relationships may be under greater environmental influences. A family history of severe class III malocclusion; abnormalities of tooth number and form; and ectopic dental development should be considered when planning treatment for relatives.
Cranio-facial morphology in class II and class III groups tends to have strong heritability, although the association is less clear in class I subjects. In particular, familial cephalometric studies have shown that mandibular length may be reduced, with a smaller mandibular body and retruded mandible in class II patients (Harris, 1975).
Furthermore, mandibular prognathism in monozygotic twins is six times higher than among dizygotic twins (Litton et al., 1970). A Japanese study showed that 70% of patients undergoing orthognathic surgery for class III malocclusion have a first-degree relative with mandibular prognathism (Watanabe et al., 2005). Therefore, a history of orthognathic intervention in a family member should be considered when planning early treatment and anticipating future growth in class III malocclusion.
There is also a familial link in relation to supernumerary teeth. Inheritance does not follow a simple Mendelian pattern, being variously described as an autosomal dominant trait with incomplete penetrance, a sex-linked trait and an autosomal recessive trait with lesser penetrance in females (Fleming et al., 2010). Hypodontia has also been linked to specific mutations related to MSX1 and PAX9 genes, and tends to co-exist with microdontia (Brook, 1984). Genetic factors are also implicated in palatal impaction of maxillary canines; dental transpositions; infra-occlusion of primary molars; and impaction of first permanent molars.
Genetic susceptibility to severe root resorption during orthodontic treatment has also been attributed to mutations of genes encoding interleukin-1 beta (IL-1β). Consequently, the potential for extensive resorption should be anticipated in family members. Treatment objectives may be modified accordingly.
Medical History
A comprehensive medical history should be taken for each patient. Whilst there are few medical conditions that contraindicate orthodontic treatment in a compliant dentally fit individual, several can impact on the delivery of care.
Heart Defects with Risk of Infective Endocarditis
Infective endocarditis is a rare cardiac condition with mortality rates of up to 40%. Previously, antibiotic prophylaxis was recommended for patients with structural heart defects predisposing to formation of valvular vegetations, which may culminate in infective endocarditis. High-risk conditions include previous infective endocarditis, prosthetic heart valves and acquired valvular disease with stenosis or regurgitation. However, under new National Institute of Health and Clinical Excellence (NICE) guidelines in the UK, the use of prophylactic antibiotics is no longer recommended for dental procedures (NICE, 2008).
Is Antibiotic Cover Required Prior to Any Orthodontic Procedure?
Historically, antibiotic cover has been recommended for dental procedures involving gingival manipulation on patients with structural defects of the heart. The rationale for use of antibiotics was to counteract transient bacteraemia that may lead to infective endocarditis. Susceptible orthodontic procedures included placement of separators and bands, and removal of appliances. However, NICE now advises that use of prophylactic antibiotics is not indicated (NICE, 2008). The cost-efficacy of prophylaxis is unproven. The use of antibiotics has a reported attendant morbidity with fatal anaphylaxis of up to 12–25 cases per million (Ahlstedt, 1984). This risk is thought to outweigh the benefits of their use. Therefore, in current practice, antibiotic cover is not routinely recommended for patients with a structural heart defect undergoing orthodontic treatment.
Bleeding Disorders
Conditions such as haemophilia do not preclude orthodontic treatment; however, treatment should involve haematological input. These patients are also at higher risk of carrying blood-borne viral infections, including HIV or hepatitis.
How Will His History of haemophilia A Affect His Management?
Oral Hygiene
Prior to instituting treatment, the importance of excellent oral hygiene should be emphasized. This may necessitate sessions with a dental hygienist or oral hygiene educators. A plaque score below 10% should be achieved before committing to treatment.
Treatment Planning
If possible treatment should be undertaken on a non-extraction basis, obviating the risks of extractions and complex haematological management of extractions. Space creation may therefore be achieved by arch lengthening involving transverse or anteroposterior arch expansion or by inter-proximal reduction.
Management of Extractions
Where extractions are necessary, these should be managed with input from physicians. Factor VIII production may be increased with 1-desamino-8-D-arginine vasopressin (DDAVP). Cryoprecipitate, Factor VIII in isolation or fresh frozen plasma may be used to replace missing Factor VIII. An anti-fibrinolytic, tranexamic acid, is also useful to stabilize clot formation.
Gingival Trauma and Soft Tissue Irritation
Efforts should be made to make the appliance as safe and unobtrusive as possible. In particular, wire ligatures should be avoided and use of self-ligating brackets can be considered. Soft tissue trauma from sharp and long wire ends should be avoided.
Allergies
The most important allergies in relation to orthodontic treatment are those associated with exposure to latex and nickel. Hypersensitivity reactions occurring with either allergen may be immediate (Type I) or delayed (Type IV); however, those related to nickel are typically Type IV reactions. Type I sensitivity is antibody mediated and may present as a localized urticaria or as anaphylaxis. Type IV hypersensitivity typically results in localized allergic contact dermatitis.
Latex Allergy:
Allergy to natural rubber latex is becoming increasingly prevalent with powdered gloves harbouring latex allergens. Individuals susceptible to allergic reactions include atopic individuals with allergic rhinitis, asthma and eczema; and patients with spina bifida.
How Should Potential Orthodontic Patients with Suspected Latex Allergy Be Managed?
- Definitive diagnosis: Latex allergy can be diagnosed with either patch testing or pin prick testing, although the latter is more reliable.
- Staff training and communication: Staff should be aware of emergency protocols for dealing with anaphylactic reactions and auxiliary staff should be aware of the diagnosis.
- Appointment and surgery management: Appointments should be scheduled for the early morning with use of a latex-screened area to segregate latex-free products to avoid contamination.
- Appliance design and handling: The use of latex products should be avoided. Latex-containing gloves should be replaced with alternatives, including nitrile or vinyl. The use of elastomeric ties could be avoided with use of self-ligating brackets. Space closure should be undertaken with nickel–titanium coils. Where inter-maxillary elastics are required, latex-free elastics can be used, although they are subject to greater force degradation.
Nickel Allergy:
Nickel allergy is relatively common, affecting over 10% of females (Nielsen and Menne, 1993). Typically, Type IV hypersensitivity reactions present on the skin as contact dermatitis; however, intra-oral manifestations are less common. There appears to be a higher threshold nickel concentration required intra-orally to induce a reaction. Nickel–titanium archwires and auxiliaries, and stainless steel products, including archwires, brackets and headgear, all contain nickel. Hence, vigilance should be exercised when using these materials in at-risk patients.
What Is the Recommended Protocol in a 25-Year-Old Female Patient with a Suspected Nickel Allergy?
- Definitive diagnosis: Patch testing may be performed by a dermatologist to confirm the diagnosis.
- Treatment: Consideration could be given to use of nickel-free brackets, e.g. ceramic, gold, titanium or polycarbonate brackets. The use of nickel–titanium archwires should be avoided where intra-oral signs of a reaction are noted. These wires may be replaced by fibre-reinforced composite wires, stainless steel wires with reduced nickel content, titanium molybdenum alloy or titanium niobium wires. Rarely, in severe cases, consideration could be given to the use of clear plastic aligners.
Diabetes
Poorly controlled diabetics are more susceptible to periodontal breakdown. Excellent oral hygiene therefore needs to be maintained during orthodontic treatment.
Immunosuppression
Certain immunosuppressive drugs such as cyclosporin can cause gingival hyperplasia or drug-induced gingival overgrowth in the presence of good oral hygiene (Figure 1.4). Again, excellent oral hygiene is imperative for these patients throughout treatment, as gingival swelling may become more marked with poor plaque control (Figure 1.5).
Epilepsy
Epilepsy is a common neurological condition, occurring in 2–5% of individuals. It is considered active if a patient is taking medication or has had a seizure within the last 2 years. If treatment is to be considered, the condition should be well-controlled. Removable appliances are best avoided in epileptics as displacement of the appliance during a seizure risks airway compromise. Consequently, fixed functional appliances or class II correctors are preferred to removable alternatives. Anti-convulsants, including phenytoin, may result in gingival hyperplasia, with 50% of individuals affected within 3 months of commencing the medication. Second-line medications, including carbamazepine, may result in glossitis, xerostomia or oral ulceration.
Childhood Malignancy
Childhood malignancy and its treatment may have significant implications for orthodontic treatment. The most common malignancy is leukaemia, with acute lymphoblastic leukaemia accounting for 25% of childhood tumours. Treatment of acute leukaemia may involve bone marrow transplantation or chemotherapy. Immunosuppressants and total body irradiation are used following bone marrow replacement to prevent graft-versus-host disease.
Treatment of malignant disease in childhood with either radiotherapy or chemotherapy can result in either tooth agenesis or root shortening. Other tumours of the head and neck requiring early radiotherapy may include retinoblastoma and sarcomas.
What Side Effects of Head and Neck Radiotherapy Are of Relevance to Orthodontics?
- Root shortening and arrested tooth development
- Reduced growth hormone production and impaired bone growth: This may result in reduced craniofacial dimension
- Reduced bone density
- Mucositis
- Arrested root development
- Premature apical closure
- Microdontia
- Hypodontia
- Delayed dental development
- Enamel defects
(Sheller and Williams, 1996)
What Are the Orthodontic Implications of Childhood Malignancy and Its Treatment?
- Premium on excellent oral hygiene
- Use of light forces
- Early termination of treatment
- Consideration of compromised treatment
- Relevant medications
Bisphosphonates
Bisphosphonates inhibit the resorption of trabecular bone by impairing osteoclastic activity to maintain bone density. They have found particular application in the management of osteoporosis, and may be prescribed to reduce hypercalcaemia following bone metastasis. Potential side effects of bisphosphonates relevant to orthodontics include osteonecrosis of the jaws, delayed eruption and retarded tooth movement. Cessation of the medication is likely to be of little benefit due to the protracted half-life of some bisphosphonates, with alendronate having a half-life of 10 years.
While osteonecrosis is a serious potential consequence, it is rare, being more likely with IV administration and prolonged use. Nevertheless, care should be taken to reduce its likelihood.
How Will Her Medical History affect Her Management?
Bisphosphonates pose two major risks to her treatment. There is a very small but serious risk of developing osteonecrosis of the jaws and tooth movement is likely to be difficult. Consequently, informed consent is important prior to embarking on treatment; it is also wise to discuss treatment with the patient’s physician. As alendronate has a long half-life, temporary discontinuation is ineffective.
It is wise to avoid invasive procedures, including extractions or temporary anchorage devices. If required, space may be created by transverse or anteroposterior arch expansion or inter-proximal reduction. Alternatively, the goals of treatment can be modified to accept a compromised outcome, obviating the need for extractions and reducing the overall treatment time. In addition, great care should be taken to ensure appliances are smooth and well-fitting, limiting the risk of ulceration and soft tissue trauma. Occasionally, orthodontics is best avoided with a restorative approach being an alternative.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs may be used on a long-term basis for chronic illness, including rheumatoid arthritis. They are also recommended for analgesia following manipulation of orthodontic appliances. They act by inhibiting cyclo-oxygenase activity, inhibiting production of prostaglandins. Animal studies have suggested that use of NSAIDs, including aspirin and ibuprofen, for pain control may retard tooth movement (Arias and Marquez-Orozco, 2006). Nevertheless, as their analgesic properties are proven, they continue to have application in orthodontic pain control.
Clinical Examination
Orthodontic treatment planning decisions are governed by both facial and occlusal goals with the aims of optimizing facial harmony and dental aesthetics, and creating a healthy and stable occlusion both in centric relationship and in function. More specifically, treatment planning decisions, including extraction and anchorage requirements, also need to take account of intra-arch features, including degree of crowding, spacing, canine angulation and occlusal curves in relation to the tooth movements planned to achieve the treatment aims. In addition, the influence of inter-arch features in all three spatial planes has a significant bearing on treatment decisions. These features may then be amalgamated in formal space planning to make robust and consistent treatment plans.
Extra-Oral Examination
The face should be examined both at rest and in animation from the front and in profile. Although absolute measurements can be made and compared to anthropometric means, of more importance are the proportions of component parts relative to each other. Any areas of disproportion should be noted.
What Is Natural Head Posture and Why Is It Important?
Natural head posture is the physiological position in which the head is held during normal function. During clinical and cephalometric examination, the orthodontist tries to replicate this using natural head position. This can be reproduced by asking the patient to look straight ahead into the distance, or look at themself in a mirror placed in front of them at eye level. Natural head position has been shown to be remarkably reproducible, allowing the orthodontist to compare the soft and hard tissues to an extra-cranial true vertical reference line. This avoids reliance on intra-cranial planes for reference, which are not only subject to significant biological variability but also the same distortion as the facial skeleton in the presence of anomalies of skeletal growth.
Frontal View:
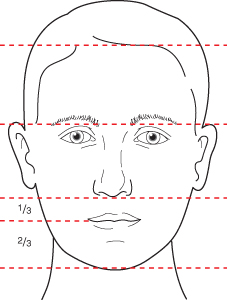
- Vertically: The face can be divided into thirds. The lower face can be divided further into thirds with the lower lip making up two-thirds and the upper lip one-third of the total (Figure 1.6).
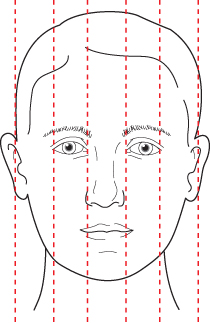
- Transversely: The face can be divided into fifths, with each fifth being approximately the width of the eye (Figure 1.7). Any asymmetry should be noted.
The patient’s lips are described as:
- Competent when they meet at rest
- Incompetent when they are apart at rest.
Lip incompetence occurs due to either anteroposterior skeletal discrepancy or increased vertical skeletal proportions. The amount of maxillary incisor display at rest should be approximately 3–4 mm in males and 4–5 mm in females in late adolescence and early adulthood. Incisor show decreases with age, although over 90% of upper lip length is established in females by the age of 7 years (Nanda et al., 1990). Lip competence tends to increase with maturation of the soft tissues and increasing social awareness in adolescence.
What Factors Contribute to an Attractive Smile?
Smiling is an integral part of human communication and one of the principal aims of orthodontics is to create a pleasing smile. The patient should therefore be examined in animation during smiling (Sarver, 2001). The three areas that need to be assessed are:
- Vertical incisor position: On smiling, most of the upper incisor should be displayed but without excessive gingival display. However, the amount of tooth and gingival display decreases with maturation; this should be borne in mind when examining a younger patient. The gingival contour of the maxillary anterior teeth should also be assessed, the gingival margins of the central incisors and canines ideally being slightly higher than the lateral incisors.
- Smile width: The width of the maxillary arch in relation to the lips should be assessed. If the arch is too narrow or set back, the space between the buccal dentition and angle of the mouth, known as the buccal corridor, can be excessive, making the arch look narrow. However, some space to frame the smile is important; otherwise the smile can look artificial. Arch expansion, appropriate torque in the buccal segments, as well as the anteroposterior position of the maxilla relative to the lip drape influence the size of the buccal corridors (Isiksal et al., 2006).
- Smile arc: On smiling the incisal edges of the upper anterior teeth should lie on the arc of the lower lip. This is called a consonant smile and is considered the most pleasing (Frush and Fisher, 1958). If the upper anterior teeth follow a straight line, the smile can also look artificial.
Profile View
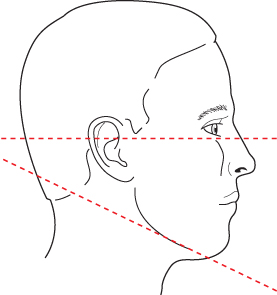
- Vertically: The face can also be divided into equal thirds. The angle between the lower border of the mandible and the Frankfort horizontal plane can be measured with imaginary lines intersecting at the occiput in the presence of a normal vertical relationship (Figure 1.8).
- Anteroposterior: The relative position of the dental bases should be described in relation to the cranial base and to each other. These can be visualized by direct palpation or by dropping a vertical line from the forehead through the intersection of the upper lip and base of nose (subnasale) (Figure 1.9). The upper lip should rest on or slightly in front of this line, whilst the chin point should be just behind it. The maxillary dental base should lie approximately 4 mm in front of the mandibular dental base.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses