1
An Appraisal of the Complete Denture Situation
Total tooth loss
Perhaps the most fundamental question to ask in the first chapter of a book on complete dentures is: ‘What is the demand for such treatment?’ Fortunately, more and more evidence has become available to provide an increasingly accurate answer and one which enables future trends to be determined with reasonable confidence. Particularly notable are the series of in-depth studies of adult dental health in the UK that have succeeded in painting a detailed picture over a period of more than 30 years. There are also data from Sweden and Finland and parts of Germany that allow some statistical modelling of the current trends (Mojon et al. 2004).
The most detailed picture comes from the UK and the information that follows is based upon decennial surveys, the most recent one undertaken in 1998.
The situation at the end of the twentieth century
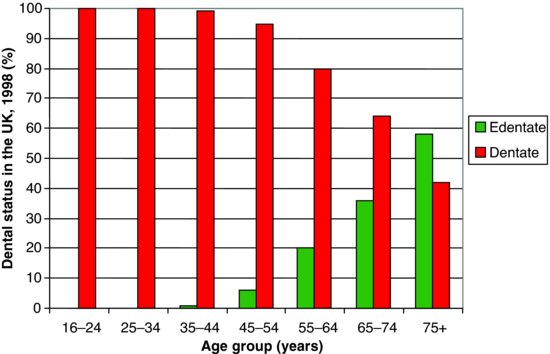
Whilst we await the publication of the survey outlining the state of adult dental health during the first decade of the twenty-first century, let us first look at total tooth loss within adults in the UK in 1998 (Fig. 1.1) (Steele et al. 2000). Overall, 13% of all adults were edentate, and it can be seen that the condition was strongly correlated with age. Total tooth loss was a rarity up to the mid-forties age group, after which there was a steady climb to the age group 75 and over where the majority had lost all their teeth.
Total tooth loss is related not only to age but also to other variables such as social class and marital status. When multivariate analyses were undertaken, any association between tooth loss and gender disappeared. The differences that are apparent in the UK may be illustrated by comparing extremes. To quote from Steele et al. (2000), women from an unskilled manual background living in Scotland were 12 times more likely to have no teeth at all than men from a non-manual background in the south of England. Of those who had lost their remaining teeth in the previous 10 years, 59% stated that they visited the dentist only when troubled whilst 29% said that they had attended their dentist on a regular basis. This pattern of attendance was almost the complete opposite to that of people who still had their own teeth. What is of particular relevance is the change in the rate at which people lost their remaining teeth in the last 10 years of the twentieth century. It has been a much more gradual process than previously. Whereas in 1968 two-thirds of those who were rendered edentulous had 12 or more teeth extracted at the final stage, in 1998 the proportion had gone down to one-quarter. One possible reason for this change is that both patient and dentist wanted to keep some natural teeth for as long as possible. We are fully supportive of this philosophy and enlarge on the topic of transition from the natural to the artificial dentition in Chapter 3.
Figure 1.1 The proportion of dentate and edentate people, by age, in the UK in 1998 (with acknowledgements to Steele et al. (2000)).
As people increasingly wish to function with their natural teeth rather than with dentures, one would expect mental barriers to be erected against the latter. This indeed appears to be the case when we consider that, in 1998, over 60% of those people who relied only on natural teeth stated that they would be very upset if they had to function with complete dentures. This attitude seems to have strengthened as we have moved into the twenty-first century. As the number of edentate patients falls, a ‘tipping-point’ appears to have been established, which results in a range of concerns being raised, including the social acceptability of being edentulous. Whilst edentulism was previously thought to be almost inevitable, and thus an ‘acceptable’ option for patients with dental disease, this is no longer the case in many areas of society. As the number of edentulous patients falls, this smaller population becomes more manageable and allows the possibility for this group of people to be offered other treatments. For example, when there is little chance of maintaining a functional natural dentition, first-line treatment options have increasingly moved towards the preservation of some tooth roots and the use of overdentures. When this is not possible, then the use of implant-supported overdentures as the ‘standard of care’ has been proposed (Feine et al. 2002; Thomason et al. 2009).
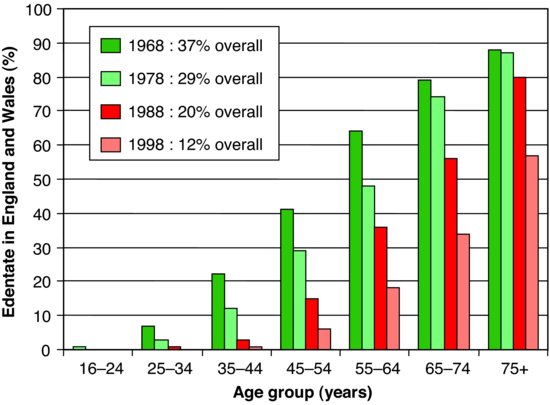
Figure 1.2 The relationship of total tooth loss to age over the period 1968–1998 (with acknowledgements to Steele et al. (2000)).
These changes of emphasis on how one may manage the progression from the dentate state to complete dentures are important, especially as most of the complete denture treatment in the future will inevitably be undertaken on older patients. It is imperative that the dentist is aware of the various treatment opportunities, of the need to explore acceptable alternatives and to move into much longer-term treatment planning whilst the patients still have a functional dentition. This longer-term planning may be best regarded as treatment ‘mapping’ as the absolute plan may need to be more flexible than is commonly the case in many treatment plans.
The past
So much for the ‘snap-shot’ of total tooth loss in 1998. A fascinating picture emerges when examining the trends that have developed over the 30-year period during which there have been four studies of adult dental health in England and Wales – 1968, 1978, 1988 and 1998. The relationship of total tooth loss to age is presented in Fig. 1.2. The first point to make is that dental health, as measured by total tooth loss, has improved dramatically. In 1968, 37% of adults in England and Wales had lost all their natural teeth. This figure had gone down to 12% in 1998. This improvement reflects the poor state of oral health before and after World War II when the main thrust of treatment, at the inception of the UK’s National Health Service, had to be an attack on the high levels of neglect, pain and sepsis existing in the community. Once this battle was won, the pattern of extractions and dentures gave way to a desire to restore the teeth and, eventually, to prevent further disease. We are perhaps now seeing the next phase where alternatives and longer-term strategies of management and rehabilitation of what remains can be realistically considered.
The very high percentage of those aged 75 and over who had lost all their teeth at the time of the earlier surveys (Fig. 1.2) is of course a reflection of the high levels of dental disease many years earlier. For example, in 1968, 64% of all those in the age group 55–64 were edentate. That same group of people continued to lose their natural teeth until, 20 years later, 80% of them (now in the 75 and over age group) were edentate.
Referring again to Fig. 1.2, we can see how the huge improvement in oral health of the younger members of the population a few years ago is now influencing the figures as these people enter their middle years. Looking again at the 55–64 age group the percentage that had lost all their teeth has dropped from 64% in 1968 to 18% in 1998. More dramatic still is the reduction in the 45–54 age group – down from 41% to 6% in the same period. As these people grow older, it is reasonable to expect that they will, in 20–30 years time, bring down a lot further the current 57% of those 75 and over who are edentate.
The future
With the mass of information which has been accumulated over the last 30 years, it has become possible to predict future trends with reasonable confidence. If the current trends continue, it is calculated that, by 2018, only 5–6% of the UK adult population will be edentate; let us not forget, though, that 5–6% equates to four million people in the UK. We will need to wait for the results of the 2008–2009 UK Adult Dental Health Survey to see if the UK is still on course for these predicted improvements. On a more salutary note, it has been suggested that the effect of having an ageing population will mitigate against the rate of reduction in the overall prevalence of edentulism in the population. Indeed, in the US it has been predicted that far from decreasing, the need for complete denture treatment will actually increase over the first 2 decades of the twenty-first century (Douglass et al. 2002). The authors argue that the ageing ‘baby boomers’ will more than compensate for the falling prevalence of edentulism. Modelling these changes on European data has suggested that in the UK there will be a reduction in edentulism of the order of 60% over the first 30 years of the century, but it will then remain stable. The mean prediction for Finland follows a similar picture to the UK but the spread of the data is very wide and so is inconclusive (Mojon et al. 2004).
Total tooth loss in other countries
An investigation into the oral health of adults in the Republic of Ireland was undertaken in 1989–1990 (O’Mullane & Whelton 1992). The level of total tooth loss was very similar to that in England, Wales and Northern Ireland in 1988. There had been a considerable decline in the level of edentulousness compared with 10 years earlier.
The relationship of total tooth loss to age is a worldwide phenomenon, as shown in Table 1.1, where the percentage of edentulous individuals for two age groups in a number of countries is shown. The amount of total tooth loss recorded in or around 1990 varies considerably between countries (WHO 1992). Whilst most EU countries do not have national survey data, in France a recent survey in the region Rhone-Alpes reported that in 1995, 16% of the 65–74 age-band was edentulous compared with 36% for the UK and 34% for the region of Pomerania in Germany (Mojon et al. 2004).
Table 1.1 The percentage of people aged 35–44 years and 65 years and over with no natural teeth (data from WHO (1991)).
| Country | 35–44 years | 65+ years |
| Albania | 3.7 | 69.3 |
| Czechoslovakia | 0.7 | 38.3 |
| Denmark | 8.0 | 60.0 |
| Finland | 9.0 | 46.0 |
| Ex-GDR | 0.5 | 58.0 |
| Germany, Federal Republic | 0.4 | 27.0 |
| Hungary | 0.3 | 30.0 |
| Ireland | 4.0 | 49.0 |
| Italy | 0.3 | 18.0 |
| The Netherlands | 9.4 | 65.4 |
| Norway | 1.0 | 31.0 |
| Romania | 15.0 | 55.8 |
| San Marino | 1.3 | 40.7 |
| Sweden | 1.0 | 20.0 |
| Turkey | 2.7 | 75.0 |
| United Kingdom | 4.0 | 67.0 |
| (Former) Yugoslavia | 0.6 | 33.0 |
The prospects for the future may be summarised as follows:
- It is unlikely that the edentulous state will disappear, but there probably will be a fall in those requiring complete dentures so that there will be around 60% of the current number required.
- More people will retain a functional natural dentition into old age, but this dentition will not last a lifetime in all cases.
- As the public’s expectations for oral health continue to rise, a larger proportion of those who lose their teeth will be very upset about the prospect of having to wear complete dentures and this will influence their response to treatment. Therefore, it will be critical to consider alternative treatment strategies for these patients.
- Most complete denture treatment will be centred on older people and is, therefore, likely to become more complex and demanding. The opportunities to consider retaining teeth as overdenture abutments or to provide osseointegrated implants as overdenture abutments for this group of patients are likely to increase and decisions will have to be made at an appropriate time in the planning cycle.
- Dentists will continue to need complete denture skills, which will have to be of a high order (Steele et al. 2000). Nevertheless, there will be less opportunity for the majority of dentists to practice these skills on a regular basis and some parts of this treatment provision are likely to move into the realm of the specialist.
In the remainder of this book, we endeavour to deal with all these points.
The limitations of complete dentures
The limitations of complete dentures are highlighted when one compares the difference between functioning natural teeth, intimately connected to and embedded in living tissues, with the removable prosthesis which replaces them, constructed of an artificial material simply resting on vital living (and often delicate) tissues. Between these two extremes is the complete overdenture. Whilst having many of the characteristics of the conventional complete denture, it retains elements of functioning teeth in the form of roots. These roots retain a vital periodontal organ and are, therefore, intimately attached to and function with the alveolar bone. Support is provided through this intimate link with the rest of the body and retention can be provided through the use of attachments between the root surfaces and the prosthesis. A similar and better researched area of clinical practice is the use of the dental implant which provides support and retention for the complete overdenture. Clearly, once teeth have been extracted, the use of implants is the only way that overdentures can be made. However, before the last teeth are extracted, both treatment options remain available and the use of natural teeth as overdenture abutments is certainly a less expensive alternative than the implant-supported prostheses.
The resorption and prosthetic replacement of alveolar bone
It is of fundamental importance to remember that the extraction of teeth does not simply mean the loss of the visible crowns. With the loss of the roots, the surrounding alveolar bone resorbs. Whilst it is relatively simple to provide an effective replacement for the natural crowns with a denture, it is frequently difficult, or even impossible, to make good all the lost alveolar bone; the more bone that is resorbed, the greater is the problem.
Atwood (1971) described the continuing resorption of the residual ridges as ‘a major oral disease entity’. It occurs in all edentulous patients and proceeds throughout life. Indeed, this would be a major argument in itself for retaining tooth roots as overdenture abutments in that their very presence will reduce the amount of alveolar resorption.
There is, though, considerable individual variation with respect to both amount and rate of loss of bone. Much has been written on the subject, and there has been a comprehensive review of the literature by Carlsson (1998). A single dominant factor responsible for ridge resorption has not yet been found. There are contradictory reports from investigations into the link between bone resorption and such factors as gender, duration of edentulousness, denture-wearing habits, quality of dentures and systemic influences.
Figure 1.3 (a) This complete lower denture covers only a small proportion of the available denture-bearing tissue and (b) as a consequence there has been increased resorption of bone and the imprint of the denture can be seen clearly.
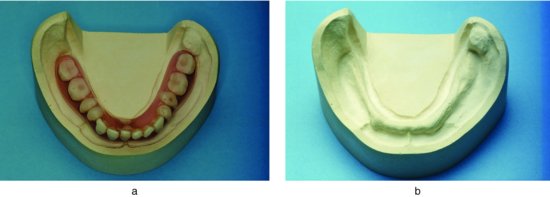
What does emerge is an explanation that, in the early stages of edentulousness, the shape of the residual ridge and the amount of resorption is likely to be influenced particularly by local factors such as the inherent quality and size of the ridge, the technique used to extract the teeth, the healing capacity of the patient and the loads applied to the ridge (Xie et al. 1997a). An example of the latter is shown in Fig. 1.3a, where it can be seen that the lower denture covers only a small part of the area available to support it and, therefore, is not spreading the load sufficiently. This design error results in increased functional stress. The consequence is seen in Fig. 1.3b, where the imprint of the border of the denture can be seen on the residual ridge; the bone has resorbed and the denture has sunk into the underlying tissues. The ‘sinking’ denture illustrates one of the fundamental advantages of the use of an overdenture compared with a conventional complete denture. Although there has been little conclusive research in this area, it is clinically apparent that supporting complete dentures on tooth remnants as overdentures reduces bone resorption. This may be assumed to be by transferring the usual compressive load of the denture through the mucosa into a tensional load within the periodontium.
It is suggested that the later stages of resorption in the edentulous are likely to be influenced more by systemic factors such as age, nutrition, drug therapy (e.g. corticosteroids) and hormonal factors. There is also a view that severe resorption, particularly of the mandible, is influenced more by systemic factors than by local factors (Xie et al. 1997b).
In spite of the gaps in our knowledge, there would seem to be a sensible way forward. Bearing in mind that a good foundation for complete dentures is such a valuable commodity, and that this foundation is capable of being damaged, it is important to take simple practical steps to reduce the risk. Therefore, the first step to be considered is maintaining some of the last few tooth roots prior to committing a patient to conventional complete dentures. Where this is not possible (and the use of implants as overdenture abutments is precluded), it is wise to encourage patients to reduce the loads on the denture-bearing tissues by leaving at least the lower denture out when sleeping, and to ensure that there is no error in denture design which would promote undue resorption. Regular recall and maintenance are also very important so that any developing problems are identified at an early stage before serious damage has been done. All these factors are highlighted elsewhere in this book.
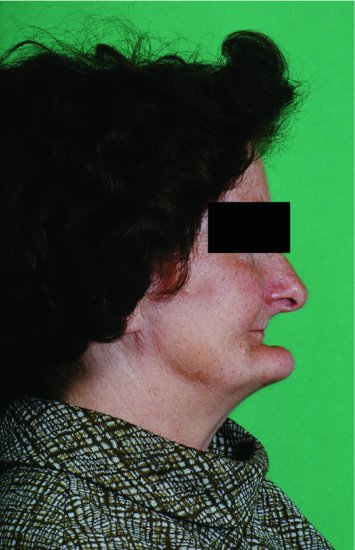
The radiograph reproduced in Fig. 1.4 is an example of extreme resorption; in simple terms, the mandible can be described as ‘pencil-thin’. With the loss of skeletal bone comes the loss of support for the facial muscles resulting in the appearance seen in Fig. 1.5. It will be appreciated that to make good this huge volume of lost teeth and bone requires very large dentures. It can become very difficult for the patient to control such substantial foreign bodies. Having lost the opportunity to reduce the resorption by retaining some tooth roots at an early stage of treatment planning, the practical opportunity to avoid further bone loss by the use of osseointegrated implants may also have been lost, as the amount of resorption may no longer leave enough bone into which to place the implants. These plans need to be considered early in the planning cycle to be of maximum benefit.
Figure 1.4 This orthopantomograph shows excessive resorption, particularly of the mandible.
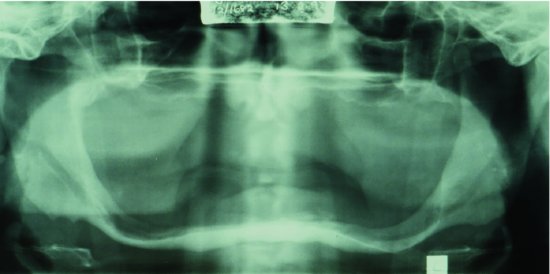
Figure 1.5 Excessive resorption of both jaws has resulted in a dramatic collapse of the lower portion of the face.
Restoration of appearance
The limitations of complete dentures in restoring tissue loss, and thus supporting the lips and cheeks fully, can contribute to an appearance of premature ageing in the edentulous patient (Fig. 1.6). The facial muscles may lose some of their tone through the ageing process, but loss of tone may also occur because the muscles are unable to function as effectively as before. This is because the underlying artificial supports (the dentures) are only sitting on the mucosa and are not attached securely to the rest of the facial skeleton. In fact, one can liken the difference in oral function between dentate and edentate individuals to that of a person striding briskly along a path rather than moving gingerly over a sheet of ice. The fact that the muscles need a stable surface over which to function further strengthens any arguments in favour of the use of overdenture abutments whether as natural tooth overdenture abutments or in the form of dental implants. A series of studies from McGill University compared patient satisfaction with implant-supported overdentures compared with conventional dentures. Typically, scores for satisfaction with stability o/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


