Transcutaneous Approaches Through the Lower Eyelid
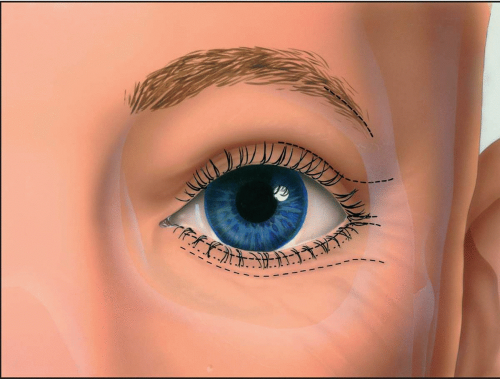
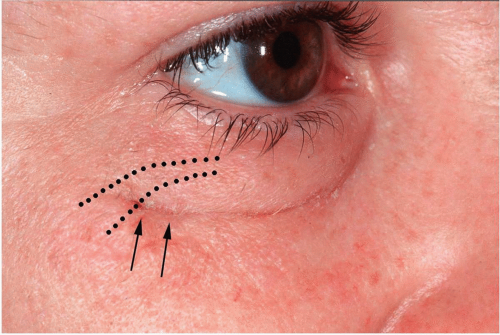
Approaches through the external side of the lower eyelid offer superb exposure to the inferior orbital rim, the floor of the orbit, the lateral orbit, and the inferior portion of the medial orbital rim and wall. These approaches are given many names in the literature (e.g., blepharoplasty, subciliary, lower- or mid-eyelid, subtarsal, infraorbital rim), based primarily on the position of the skin incision in the lower eyelid. Because of the natural skin creases in the lower eyelid and the thinness of eyelid skin, scars become inconspicuous with time and do not form keloids. The infraorbital incision, however, is almost always noticeable to some degree (see Fig 2.1).
SURGICAL ANATOMY
Lower Eyelid
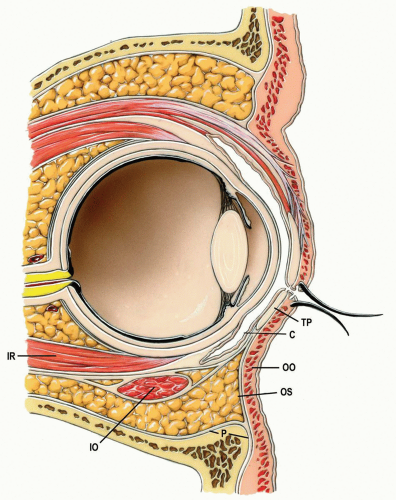
In the sagittal section, the lower eyelid (1) consists of at least four distinct layers: the skin and subcutaneous tissue, the orbicularis oculi muscle, the tarsus (upper 4 to 5 mm of the eyelid) or orbital septum, and the conjunctiva (see Fig. 2.2).
Skin
The skin is the outermost layer, and comprises the epidermis and the very thin dermis. The skin of the eyelids is the thinnest in the body and has many elastic fibers that allow it to be stretched during dissection and retraction. It is loosely attached to the underlying muscle; therefore, in contrast to most areas of the face, relatively large quantities of fluid may accumulate subcutaneously in this loose connective tissue. The skin derives its blood supply from the underlying perforating blood vessels of the muscles (see subsequent text).
Muscle
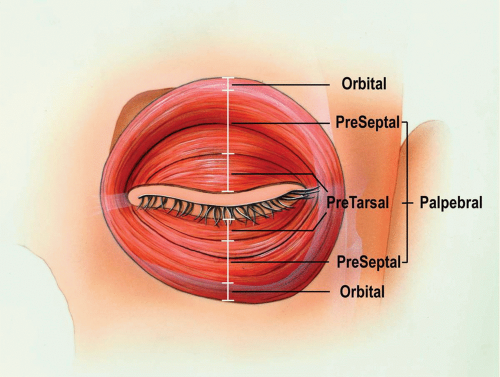
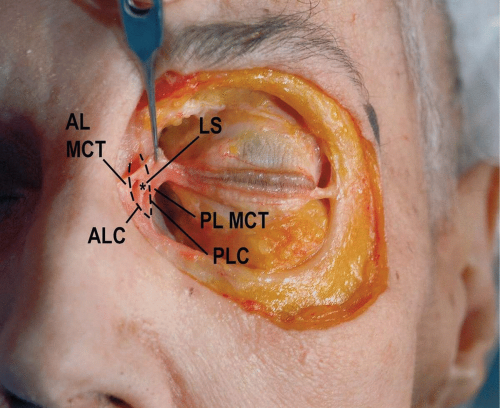
The orbicularis oculi muscle, the sphincter of the eyelids, lies subjacent and adherent to the skin (see Fig. 2.3). This muscle completely encircles the palpebral fissure and extends over the skeleton of the orbit. It can therefore be divided into orbital and palpebral portions (see Fig. 2.4). The palpebral portion can be further subdivided into the pretarsal portion (i.e., the muscle superficial to the tarsal plates) and the preseptal portion (i.e., the muscle superficial to the orbital septum). The palpebral portion of the orbicularis oculi muscle is very thin in cross section, especially at the junction of the pretarsal and preseptal portions. The orbital portion of the orbicularis oculi muscle originates medially from the bones of the medial orbital rim and the medial canthal tendon. The peripheral fibers sweep across the eyelid over the orbital margin in a series of concentric loops, the more central ones forming almost complete rings. In the lower eyelid, the orbital portion extends below the inferior orbital rim onto the cheek and covers the origins of the elevator muscles of the upper lip and nasal ala. The orbital portion of the orbicularis oculi muscle is responsible for tight closure of the eye.
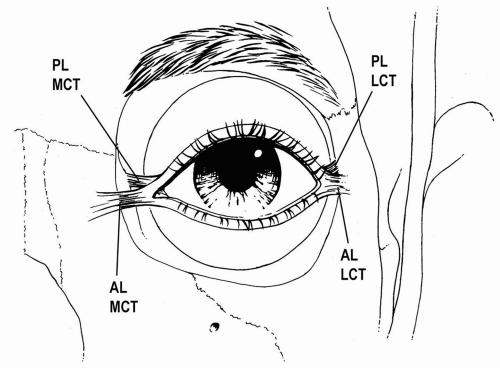
The preseptal portion of the orbicularis oculi muscle originates from the medial canthal tendon and lacrimal diaphragm and passes across the eyelid as a series of half-ellipses, meeting at the lateral canthal tendon. The upper and lower pretarsal muscles contribute to the lateral canthal tendon which extends approximately 7 mm before inserting lateral orbital tubercle. Medially, they unite to form the medial canthal tendon, which inserts on the medial orbital margin, the anterior lacrimal crest, and the nasal bones. The palpebral portion of the orbicularis oculi muscle functions to close the eye without effort, as in blinking. It also functions to maintain contact between the lower eyelid and the ocular globe.
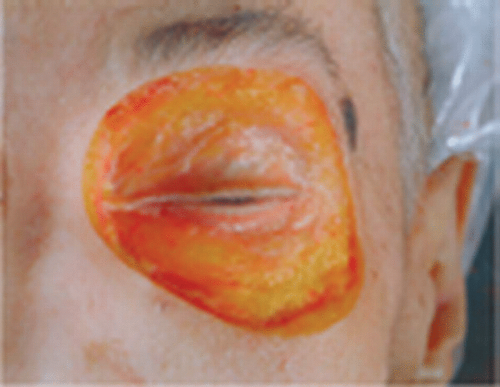
Figure 2.3 Anatomic dissection of orbicularis oculi muscle fibers. Note the extreme thinness in this older specimen.
|

Figure 2.5 Anatomic dissection of orbital septum in the lower eyelid. Note the thinness in this older specimen.
|
The orbicularis oculi muscle is innervated laterally from the branches of the facial nerve that enter the muscle on its deeper surface. The blood supply to the orbicularis oculi muscle is from the external facial artery tributaries arising from the deep branches of the ophthalmic artery. These arterial branches form a marginal arcade, traversing between the tarsal plate and the muscle and giving rise to branches that perforate the substance of the muscle, the orbital septum, and the tarsal plate.
Orbital Septum/Tarsus
The orbital septum is a fascial diaphragm between the contents of the orbit and the superficial face (Figs. 2.1 and 2.5). It is usually denser laterally than medially, but varies considerably in thickness from one individual to another, and weakens with age, allowing the orbital fat pads to bulge onto the face. The orbital septum is a fascial extension of the periosteum of the bones of the face and orbit. It originates along the orbital rim for most of its extent. Laterally and inferolaterally, however, it arises from the periosteum 1 to 2 mm beyond the rim of the orbit. Therefore, it is necessary to dissect a few millimeters lateral and/or inferior to the orbital rim before incising the periosteum to prevent incising through the orbital septum.
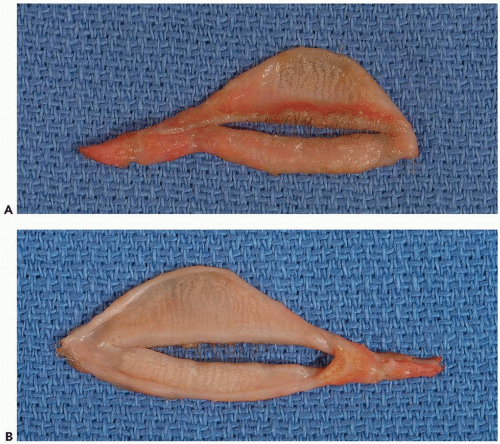
The orbital septum of the lower eyelid inserts into the inferior margin of the lower tarsus. The tarsal plate of the lower eyelid is a somewhat thin, pliable, fibrocartilaginous structure that gives form and support to the lower eyelid (see Fig. 2.6A and B). The edge of the tarsus that is adjacent to the free border of the eyelid is parallel to the palpebral fissure, whereas the deeper (inferior) border is curved such that the tarsus is somewhat semilunar in shape.
It is also, of course, curved to conform to the outer surface of the eyeball. The inferior tarsus at approximately 4 to 5 mm is half the height of the superior tarsus (approximately 10 mm). The tarsal glands, sandwiched between the layers of fibrocartilage in the lower eyelid, are smaller than their upper eyelid counterpart, and exit on the eyelid margin near the lash follicles. The lashes are supported by their roots, which are attached to fibrous tissue on the tarsal plate and not in the orbicularis oculi muscle anterior to the tarsal plate. Laterally, the tarsal plate becomes a fibrous band that adjoins the structural counterpart from the upper eyelid, forming the lateral canthal tendon. Medially, the tarsal plate also becomes fibrous and shelters the inferior lacrimal canaliculus behind, as it becomes the medial canthal tendon.
It is also, of course, curved to conform to the outer surface of the eyeball. The inferior tarsus at approximately 4 to 5 mm is half the height of the superior tarsus (approximately 10 mm). The tarsal glands, sandwiched between the layers of fibrocartilage in the lower eyelid, are smaller than their upper eyelid counterpart, and exit on the eyelid margin near the lash follicles. The lashes are supported by their roots, which are attached to fibrous tissue on the tarsal plate and not in the orbicularis oculi muscle anterior to the tarsal plate. Laterally, the tarsal plate becomes a fibrous band that adjoins the structural counterpart from the upper eyelid, forming the lateral canthal tendon. Medially, the tarsal plate also becomes fibrous and shelters the inferior lacrimal canaliculus behind, as it becomes the medial canthal tendon.
Embedded within the tarsal plates are large sebaceous glands called the tarsal or Meibomian glands, whose ducts may be seen along the eyelid margin. A grayish line or a slight groove, which is sometimes visible between the lashes and the openings of the tarsal glands, represents the junction of the two fundamental portions of the eyelid: the skin and muscle on one hand and the tarsus (the plate of closely packed tarsal glands) and conjunctiva on the other. This junction indicates a plane along which the eyelid may be split into anterior and posterior portions with minimal scarring.
Palpebral Conjunctiva
The conjunctiva that lines the inner surface of the eyelids is called the palpebral conjunctiva (Fig. 2.2). It adheres firmly to the tarsal plate, and as it extends inferiorly toward the inferior conjunctival fornix, it becomes more loosely bound. At the inferior conjunctival fornix, the conjunctiva sweeps onto the ocular globe to become the bulbar conjunctiva.
Lateral Canthal Tendon
The lateral canthal tendon, ligament, or raphe as it is frequently called, is a fibrous extension of the tarsal plates laterally toward the orbital rim (see Fig. 2.7). As will be seen in the medial canthal tendon, the lateral canthal tendon has a superficial and a deep component. The base of the ligamentous complex is “Y”-shaped and is attached to the external angle of the two tarsi (see Fig. 2.8). The two divisions diverge from the tarsi and the superficial component extends laterally just under, or intermingles with, the orbicularis oculi muscle. It continues laterally to the orbital rim and inserts into the periosteum overlying the lateral orbital rim and the temporalis fascia just lateral to the orbital rim. The superficial limb coalesces with the temporal periosteum over the lateral orbital rim. The thicker, stronger deep component of the lateral canthal tendon courses posterolaterally, inserting into the periosteum of the orbital tubercle of the zygoma, approximately 3 to 4 mm posterior to the orbital rim. The space between the two bundles of the lateral canthal tendon is filled with loose connective tissue.
Medial Canthal Tendon
The medial canthal tendon is attached to the medial bony orbit by the superficial and the deep components that attach to the anterior and posterior lacrimal crests (see Figs. 2.8 and 2.9) (2,3). The medial canthal tendon originates at the nasal border of the upper and lower tarsi, where the preseptal muscles divide into superficial and deep heads (4). The lacrimal puncta are located here. Therefore, the lacrimal canaliculi of the upper and lower eyelid margins extend from the medial border of the tarsi toward and behind the medial canthus. Continuing medially, the tendon fans out to insert into the anterior lacrimal crest and beyond onto the frontal process of the maxilla. The anterior lacrimal crest, which is 2 to 3 mm medial to the canthal apex, protects the lacrimal sac. Therefore, an incision farther medial than 3 mm from the canthus misses both the canaliculi and the sac.

Figure 2.7 Anatomic dissection of the deep portion of the lateral canthal tendon. Note that it attaches posterior to the orbital rim.
|
The anterior horizontal segment is the strongest component of the medial canthal tendon complex and is attached most firmly at the anterior lacrimal crest. The thinner posterior limb inserts into the posterior lacrimal crest and functions to maintain the eyelids in a posture tangential to the globe. The resultant vector of all the canthal attachments suggests that resuspension of the entire complex following disruption should be posterior and superior to the anterior lacrimal crest.
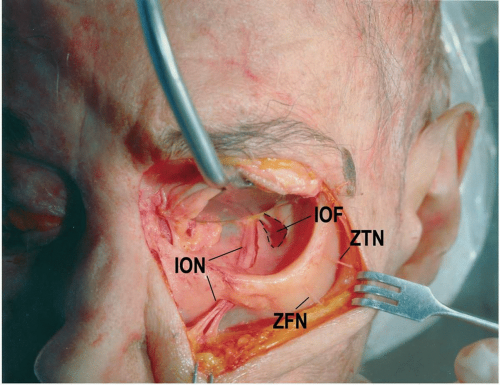
Infraorbital Groove
The infraorbital neurovascular bundle enters the posterior orbit through the inferior orbital fissure and runs almost straight anteriorly in the infraorbital groove of the orbital floor (see Fig. 2.10). More anteriorly, the infraorbital groove is usually covered with a thin layer of bone, forming the infraorbital canal, which leads the neurovascular bundle through the infraorbital foramen to the superficial structures of the face. The superior alveolar nerves split off the infraorbital nerve at a depth of 5 to 25 mm within the infraorbital canal and give sensation to the maxillary teeth and gingiva.
TECHNIQUES
Several external incisions of the lower eyelid to allow access to the infraorbital rim and orbital floor have been described. The major difference between these incisions is the level at which they are placed on the skin of the eyelid and the level at which the muscle is transected to expose the orbital septum/periosteum. Each incision has advantages and disadvantages.
The two approaches and one modification are illustrated in the following text. The first is most commonly called the subciliary incision, also known as the infraciliary or blepharoplasty incision. This incision is made just below the eyelashes. The advantages of this incision are the imperceptible scar and the ease of extending laterally for additional exposure of the entire lateral orbital rim. The second approach is usually known as the subtarsal, also known as the mid-eyelid or skin crease approach, because the incision is made lower than that in the subciliary approach, often 4 to 7 mm below the eyelid margin. The subciliary approach will be shown in great detail. The subtarsal approach will be contrasted to the subciliary approach. In addition to these approaches, a modification of the subciliary approach, which can provide access to the entire lateral rim and internal wall of the orbit, will also be illustrated.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses